Korean J Urol.
2011 Dec;52(12):858-864.
A Study Assessing the Quality of Life Related to Voiding Symptoms and Sexual Functions in Menopausal Women
- Affiliations
-
- 1Department of Urology, Inje University Busan Paik Hospital, Busan, Korea. kweonsikmin@yahoo.com
Abstract
- PURPOSE
To investigate the impact of menopause on the quality of life (QoL) of middle-aged and older women, including their general well-being, voiding-related symptoms, and sexual distress.
MATERIALS AND METHODS
To assess QoL, we administered a questionnaire that included questions about voiding-related symptoms and female sexual distress and part of the Women's Health Questionnaire. The self-administered questionnaires were completed by 1,679 women in the Korea. Data for 1,262 women were available for analysis, including premenopausal (n=307), perimenopausal (n=240), and postmenopausal (n=715) groups.
RESULTS
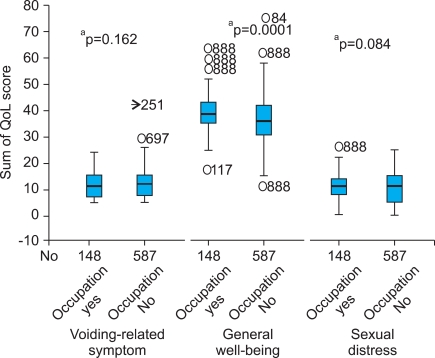
Voiding-related discomfort increased significantly in perimenopausal and postmenopausal women compared with premenopausal women (p<0.001). General well-being worsened as menopause progressed (p<0.001). Menopausal women who were older (p=0.014), had a hysterectomy (p=0.005), or had urinary incontinence (p=0.001) had more voiding-related symptoms. Hypertension (p=0.026), cardiac disease (p=0.013), and arthritis (p=0.001) resulted in significantly decreased general well-being. Women with a hysterectomy (p=0.017) and those with arthritis (p=0.004) had high sexual distress. In the menopausal group, employed women had better general well-being than did unemployed women.
CONCLUSIONS
Menopause negatively affected the QoL of middle-aged and older women because of decreased general well-being and increased voiding-related symptoms. General health, even in menopausal women, was important to maintain a better QoL. To preserve the QoL of women undergoing menopause, control of menopause and underlying disease should be considered.
MeSH Terms
Figure
Reference
-
1. Gracia CR, Freeman EW, Sammel MD, Lin H, Mogul M. Hormones and sexuality during transition to menopause. Obstet Gynecol. 2007; 109:831–840. PMID: 17400843.
Article2. Hong JE, Choi HY, Hong SJ, Chung MK, Ahn TY, Rim JS, et al. Construction of a short form BPH specific health related quality of life scale: reliablility and validity tests. Korean J Urol. 2001; 42:1270–1277.3. Lee KY, Park TJ. The quality of life in the menopausal women. J Korean Acad Fam Med. 1999; 20:894–905.4. Han C, Kim HC, Kang SH, Moon DG, Kim JJ, Choi JY. Validity and reliability of Korean version of the female sexual distress scale (FSDS). Korean J Androl. 2004; 22:68–74.5. Blakeman PJ, Hilton P, Bulmer JN. Oestrogen and progesterone receptor expression in the female lower urinary tract, with reference to oestrogen status. BJU Int. 2000; 86:32–38. PMID: 10886079.
Article6. Shenfeld OZ, McCammon KA, Blackmore PF, Ratz PH. Rapid effects of estrogen and progesterone on tone and spontaneous rhythmic contractions of the rabbit bladder. Urol Res. 1999; 27:386–392. PMID: 10550529.
Article7. Rud T. The effects of estrogens and gestagens on the urethral pressure profile in urinary continent and stress incontinent women. Acta Obstet Gynecol Scand. 1980; 59:265–270. PMID: 7191614.
Article8. Sultana CJ, Walters MD. Estrogen and urinary incontinence in women. Maturitas. 1994; 20:129–138. PMID: 7715464.
Article9. Freeman EW, Sammel MD, Liu L, Gracia CR, Nelson DB, Hollander L. Hormones and menopausal status as predictors of depression in women in transition to menopause. Arch Gen Psychiatry. 2004; 61:62–70. PMID: 14706945.10. Graziottin A, Koochaki PE, Rodenberg CA, Dennerstein L. The prevalence of hypoactive sexual desire disorder in surgically menopausal women: An epidemiological study of women in four European countries. J Sex Med. 2009; 6:2143–2153. PMID: 19453880.
Article11. Shifren JL, Braunstein GD, Simon JA, Casson PR, Buster JE, Redmond GP, et al. Transdermal testosterone treatment in women with impaired sexual function after oophorectomy. N Engl J Med. 2000; 343:682–688. PMID: 10974131.
Article12. Azadzoi KM, Siroky MB. Neurologic factors in female sexual function and dysfunction. Korean J Urol. 2010; 51:443–449. PMID: 20664775.
Article13. Sherwin BB, Gelfand MM. The role of androgen in the maintenance of sexual functioning in oophorectomized women. Psychosom Med. 1987; 49:397–409. PMID: 3615768.
Article14. Kim M, Choi H. Changes in atrophic symptoms, the vaginal maturation index, and vaginal pH in postmenopausal women treated with vaginal estrogen tablets. J Korean Soc Menopause. 2010; 16:162–169.15. Ho MH, Yip S, Bhatia NN. Lower urinary tract dysfunctions in women with diabetes mellitus. Curr Opin Obstet Gynecol. 2007; 19:469–473. PMID: 17885464.
Article16. Josefsson KA, Gard G. Women's experiences of sexual health when living with rheumatoid arthritis- an explorative qualitative study. BMC Musculoskelet Disord. 2010; 11:240. PMID: 20950461.
Article17. Cayan S, Akbay E, Bozlu M, Canpolat B, Acar D, Ulusoy E. The prevalence of female sexual dysfunction and potential risk factors that may impair sexual function in Turkish women. Urol Int. 2004; 72:52–57. PMID: 14730166.
Article18. Coyne KS, Sexton CC, Irwin DE, Kopp ZS, Kelleher CJ, Milsom I. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: results from the EPIC study. BJU Int. 2008; 101:1388–1395. PMID: 18454794.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Association between Sexual Self-Efficacy and the Quality of Life among Menopausal Women
- Comparisons of Depression, Marital Intimacy, Sexual Function and Quality of Life in Sexual Active or Inactive Groups of Post-menopausal Married Women
- Comparison of quality of life and related factors according to premature menopause using the Korea National Health and Nutrition Examination Survey (2014-2017)
- Factors influencing quality of life in post-menopausal women
- A Comparative Study on Climacteric Symptoms of Natural Menopausal Women and Artificial Menopausal Women