Korean J Urol.
2011 Jun;52(6):379-383.
Comparison of Deep Biopsy Tissue Damage from Transurethral Resection of Bladder Tumors between Bipolar and Monopolar Devices
- Affiliations
-
- 1Department of Urology, College of Medicine, Yeungnam University, Daegu, Korea. htkim@ynu.ac.kr
Abstract
- PURPOSE
Bipolar energy has recently been used for transurethral resection of bladder tumor (TURBT). Although this modality is thought to be safe, there are some controversies concerning the pathologic accuracy of the biopsy specimens. We compared clinical efficacy, safety, and pathologic characteristics of deep biopsy specimens between bipolar and monopolar devices.
MATERIALS AND METHODS
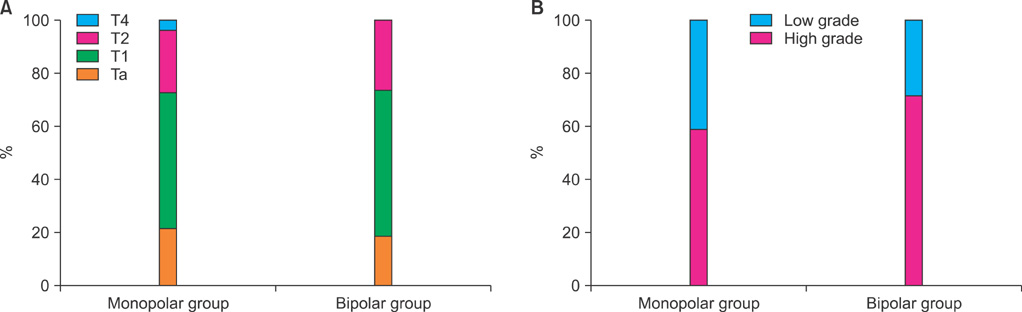
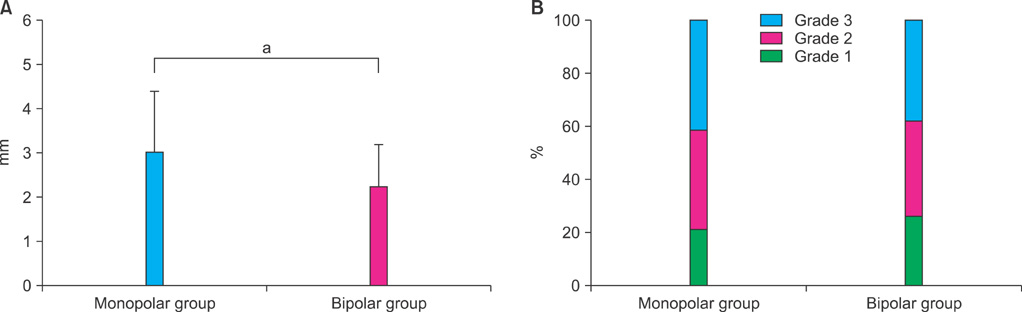
From January 2002 to June 2007, a total of 115 patients underwent TURBT with deep biopsy with the use of bipolar (bipolar group, n=64) or monopolar (monopolar group, n=51) devices. We retrospectively analyzed tumor size, tumor number, urine cytology, perioperative blood loss (postoperative changes in hemoglobin levels), complications, duration of catheterization, duration of hospitalization, pathologic stage, WHO grade, deep biopsy specimen thickness, and grade of thermal damage.
RESULTS
There were no statistical differences in tumor size, tumor number, urine cytology, complications, duration of hospitalization, pathologic stage, or WHO grade between the two groups. Postoperative changes in hemoglobin levels were significantly lower in the bipolar group (p=0.038), and the duration of catheterization was shorter in the bipolar group (p=0.026). The deep biopsy specimen thickness was significantly thinner in the bipolar group (2.25+/-0.94 mm vs. 3.02+/-1.39 mm, p<0.05). The grade of thermal damage was not statistically different between the two groups (p=0.862).
CONCLUSIONS
In terms of clinical efficacy and safety, bipolar TURBT is comparable to monopolar TURBT, having advantages in perioperative blood loss and duration of catheterization. In addition, pathologic changes in deep biopsy after bipolar and monopolar TURBT are similar. Bipolar TURBT can be properly used for bladder tumors without pathologic error.
MeSH Terms
Figure
Reference
-
1. The statistics report: the incidence of cancer on 2003-2005 and the survival rate on 1993-2005. 2009. accessed Apr 1, 2009. National Cancer Center; http://www.ncc.re.kr.2. Kim WJ, Chung JI, Hong JH, Kim CS, Jung SI, Yoon DK. Epidemiological study for urologic cancer in Korea (1998-2002). Korean J Urol. 2004. 45:1081–1088.3. Wang DS, Bird VG, Leonard VY, Plumb SJ, Konety B, Williams RD, et al. Use of bipolar energy for transurethral resection of bladder tumors: pathologic considerations. J Endourol. 2004. 18:578–582.4. Park J, Kim JB, Ahn H. Prognostic significance of the presence of proper muscle in the resected specimens of primary T1G3 bladder cancer. Korean J Urol. 2006. 47:137–142.5. Park SY, Choi HY, Lee HM. Predictive factors of advancement of the pathologic T stage after radical cystectomy in patients with clinical T2 stage bladder transitional cell carcinoma. Korean J Urol. 2007. 48:390–395.6. Balzarro M, Ficarra V, Bartoloni A, Tallarigo C, Malossini G. The pathophysiology, diagnosis and therapy of the transurethral resection of the prostate syndrome. Urol Int. 2001. 66:121–126.7. Thomas K, O'Brien T. Improving transurethral resection of bladder tumour: the gold standard for diagnosis and treatment of bladder tumours. Eur Urol. 2008. 7:Suppl. 524–528.8. Ho HS, Cheng CW. Bipolar transurethral resection of prostate: a new reference standard? Curr Opin Urol. 2008. 18:50–55.9. Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP)--incidence, management, and prevention. Eur Urol. 2006. 50:969–979.10. Issa MM. Technological advances in transurethral resection of the prostate: bipolar versus monopolar TURP. J Endourol. 2008. 22:1587–1595.11. Mamoulakis C, Ubbink DT, de La Rosette JJ. Bipolar versus monopolar transurethral resection of the prostate: a systematic review and meta-analysis of randomized controlled trials. Eur Urol. 2009. 56:798–809.12. Eaton AC, Francis RN. The provision of transurethral prostatectomy on a day-case basis using bipolar plasma kinetic technology. BJU Int. 2002. 89:534–537.13. Botto H, Lebret T, Barré P, Orsoni JL, Hervé JM, Lugagne PM. Electrovaporization of the prostate with the Gyrus device. J Endourol. 2001. 15:313–316.14. Lagerveld BW, Koot RA, Smits GA. Thermal artifacts in bladder tumors following loop endoresection: electrovaporization v electrocauterization. J Endourol. 2004. 18:583–586.15. Akgül KT, Ayyildiz A, Nuhoğlu B, Caydere M, Ustün H, Germiyanoğlu C. Comparison of transurethral prostate resection and plamakinetic prostate resection according to cautery artefacts in tissue specimens. Int Urol Nephrol. 2007. 39:1091–1096.16. Singh H, Desai MR, Shrivastav P, Vani K. Bipolar versus monopolar transurethral resection of prostate: randomized controlled study. J Endourol. 2005. 19:333–338.17. Smith D, Khoubehi B, Patel A. Bipolar electrosurgery for benign prostatic hyperplasia: transurethral electrovaporization and resection of the prostate. Curr Opin Urol. 2005. 15:95–100.18. Faul P, Schlenker B, Gratzke C, Stief CG, Reich O, Hahn RG. Clinical and technical aspects of bipolar transurethral prostate resection. Scand J Urol Nephrol. 2008. 42:318–323.19. Wendt-Nordahl G, Häcker A, Reich O, Djavan B, Alken P, Michel MS. The Vista system: a new bipolar resection device for endourological procedures: comparison with conventional resectoscope. Eur Urol. 2004. 46:586–590.20. Patel A, Adshead JM. First clinical experience with new transurethral bipolar prostate electrosurgery resection system: controlled tissue ablation (coblation technology). J Endourol. 2004. 18:959–964.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Bipolar Transurethral Resection of the Prostate: Comparison with Standard Monopolar Transurethral Resection of the Prostate
- Fluid extravasation caused by bladder perforation during bipolar transurethral resection using saline solution: a case report
- Long-term Follow-up of Bipolar Transurethral Resection of the Prostate Compared with Conventional Monopolar Resectoscope for Patients with Benign Prostatic Hyperplasia
- Bipolar Transurethral Resection of the Prostate: A Comparative Study with Monopolar Transurethral Resection
- Comparison of Effectiveness of Monopolar and Bipolar Transurethral Resection of the Prostate and Open Prostatectomy in Large Benign Prostatic Hyperplasia