Pediatr Allergy Respir Dis.
2012 Dec;22(4):404-410.
Usefulness of Pleural Adenosine Deaminase in Children for the Differentiation Tuberculous Pleural Effusion from Mycoplasma pneumonia with Pleural Effusion
- Affiliations
-
- 1Department of Pediatrics, Hanyang University Seoul Hospital, Hanyang University College of Medicine, Seoul, Korea. hablee@hanyang.ac.kr
- 2Department of Pediatrics, Hallym University Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
Abstract
- PURPOSE
Determination of adenosine deaminase (ADA) in pleural fluid has been suggested as another tool to establish early diagnosis of tuberculous pleural effusion. However, there are few studies concerning its usefulness in children. The objective of this study was to evaluate the utility of the determination of ADA level in pleural fluid for the differential diagnosis between tuberculous pleural effusion (TPE) and Mycoplasma pneumonia with pleural effusion (MP) in children.
METHODS
We retrospectively reviewed the clinical records of 13 TPE patients and 21 MP patients with pleural effusion. Also, we analyzed ADA levels, and clinical, biochemical, microbiologic and cytologic findings in the pleural fluid.
RESULTS
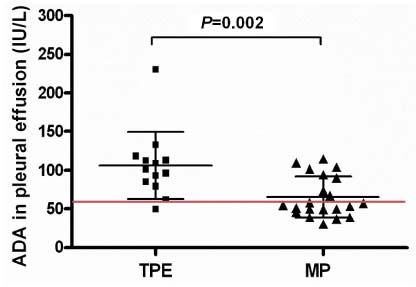
The pleural fluid of all the subjects revealed exudative rather than transudate characteristics. The mean ADA level in the TPE group was significantly higher than that in the MP group (106.27+/-43.71 IU/L vs. 65.28+/-26.27 IU/L, P=0.003). The area under the curve in receiver operating characteristic analysis was 0.810. With a cut-off level for ADA of 60 U/L, the sensitivity, specificity, positive predictive value, and negative predictive value were 92.3%, 61.9%, 60.0%, and 92.9%, respectively. As many as 38.9% of patients with MP were false-positive with this ADA cut-off setting.
CONCLUSION
Although the measurement of ADA activity in pleural fluid can help TPE diagnosis, we should consider that some cases of MP with pleural effusion showed high ADA activities. Accordingly, the utility of the ADA level in pleural fluid for the differentiation of TPE from MP declines and additional relevant studies are required.
MeSH Terms
Figure
Reference
-
1. Gopi A, Madhavan SM, Sharma SK, Sahn SA. Diagnosis and treatment of tuberculous pleural effusion in 2006. Chest. 2007. 131:880–889.
Article2. Medford AR, Maskell N. Pleural effusion. Postgrad Med J. 2005. 81:702–710.
Article3. Efrati O, Barak A. Pleural effusions in the pediatric population. Pediatr Rev. 2002. 23:417–426.
Article4. Winnie GB, Martinez FD. Behrmann RE, Kliegman RM, Jenson HB, editors. Pleurisy, pleural effusions, and empyema. Nelson Textbook of Pediatrics. 2008. 18th ed. Philadelphia: WB Saunders;954.
Article5. World Health Organization. Global tuberculosis control: WHO report 2011. 2011. Geneva: World Health Organization.6. Korea Centers for Disease Control and Prevention. Korean Institute of Tuberculosis. Annual report on the notified tuberculosis patients in Korea 2010. 2011. Seoul: Korea Centers for Disease Control and Prevention.7. Eun BW, Kim NH, Choi EH, Lee HJ. Mycoplasma pneumoniae in Korean children: the epidemiology of pneumonia over an 18-year period. J Infect. 2008. 56:326–331.
Article8. Niitu Y, Hasegawa S, Suetake T, Kubota H, Komatsu S, Horikawa M. Resistance of Mycoplasma pneumoniae to erythromycin and other antibiotics. J Pediatr. 1970. 76:438–443.
Article9. Morozumi M, Iwata S, Hasegawa K, Chiba N, Takayanagi R, Matsubara K, et al. Increased macrolide resistance of Mycoplasma pneumoniae in pediatric patients with community-acquired pneumonia. Antimicrob Agents Chemother. 2008. 52:348–350.
Article10. Peuchant O, Menard A, Renaudin H, Morozumi M, Ubukata K, Bebear CM, et al. Increased macrolide resistance of Mycoplasma pneumoniae in France directly detected in clinical specimens by real-time PCR and melting curve analysis. J Antimicrob Chemother. 2009. 64:52–58.
Article11. Chang MW, Kim KH, Park ID, Song GY, Kim SW, Lee EY, et al. Isolation of Mycoplasma pneumoniae and antimicrobial susceptibilities of the isolates(III). J Life Sci. 2005. 15:479–485.
Article12. Cha SI, Shin KM, Jeon KN, Yoo SS, Lee J, Lee SY, et al. Clinical relevance and characteristics of pleural effusion in patients with Mycoplasma pneumoniae pneumonia. Scand J Infect Dis. 2012. 44:793–797.
Article13. Valdes L, Alvarez D, Valle JM, Pose A, San Jose E. The etiology of pleural effusions in an area with high incidence of tuberculosis. Chest. 1996. 109:158–162.
Article14. Goto M, Noguchi Y, Koyama H, Hira K, Shimbo T, Fukui T. Diagnostic value of adenosine deaminase in tuberculous pleural effusion: a meta-analysis. Ann Clin Biochem. 2003. 40(Pt 4):374–381.
Article15. Giusti G. Bergmeyer HU, editor. Adenosine deaminase. Methods of Enzymatic Analysis. 1974. New York: Academic Press;1092–1099.
Article16. Lima DM, Colares JK, da Fonseca BA. Combined use of the polymerase chain reaction and detection of adenosine deaminase activity on pleural fluid improves the rate of diagnosis of pleural tuberculosis. Chest. 2003. 124:909–914.
Article17. Kroegel C, Antony VB. Immunobiology of pleural inflammation: potential implications for pathogenesis, diagnosis and therapy. Eur Respir J. 1997. 10:2411–2418.
Article18. Antony VB. Immunological mechanisms in pleural disease. Eur Respir J. 2003. 21:539–544.
Article19. Broaddus VC, Hebert CA, Vitangcol RV, Hoeffel JM, Bernstein MS, Boylan AM. Interleukin-8 is a major neutrophil chemotactic factor in pleural liquid of patients with empyema. Am Rev Respir Dis. 1992. 146:825–830.
Article20. Pace E, Gjomarkaj M, Melis M, Profita M, Spatafora M, Vignola AM, et al. Interleukin-8 induces lymphocyte chemotaxis into the pleural space. Role of pleural macrophages. Am J Respir Crit Care Med. 1999. 159(5 Pt 1):1592–1599.
Article21. Utine GE, Ozcelik U, Yalcin E, Dogru D, Kiper N, Aslan A, et al. Childhood parapneumonic effusions: biochemical and inflammatory markers. Chest. 2005. 128:1436–1441.22. Fischer D, Van der Weyden MB, Snyderman R, Kelley WN. A role for adenosine deaminase in human monocyte maturation. J Clin Invest. 1976. 58:399–407.
Article23. Barton R, Martiniuk F, Hirschhorn R, Goldschneider I. The distribution of adenosine deaminase among lymphocyte populations in the rat. J Immunol. 1979. 122:216–220.24. Piras MA, Gakis C, Budroni M, Andreoni G. Adenosine deaminase activity in pleural effusions: an aid to differential diagnosis. Br Med J. 1978. 2:1751–1752.
Article25. Burgess LJ, Maritz FJ, Le Roux I, Taljaard JJ. Combined use of pleural adenosine deaminase with lymphocyte/neutrophil ratio. Increased specificity for the diagnosis of tuberculous pleuritis. Chest. 1996. 109:414–419.
Article26. Ocana I, Martinez-Vazquez JM, Segura RM, Fernandez-De-Sevilla T, Capdevila JA. Adenosine deaminase in pleural fluids. Test for diagnosis of tuberculous pleural effusion. Chest. 1983. 84:51–53.27. van Keimpema AR, Slaats EH, Wagenaar JP. Adenosine deaminase activity, not diagnostic for tuberculous pleurisy. Eur J Respir Dis. 1987. 71:15–18.28. Maartens G, Bateman ED. Tuberculous pleural effusions: increased culture yield with bedside inoculation of pleural fluid and poor diagnostic value of adenosine deaminase. Thorax. 1991. 46:96–99.
Article29. Light R. Light RW, editor. Parapneumonic effusions and infections of the pleural space. Pleural Diseases. 1990. 2nd ed. Philadelphia: Lea&Febiger;129–149.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Utility of Pleural Adenosine Deaminase for Diagnosis of Differentiating Tuberculous Pleural Effusion in Children
- A Case of Mycoplasma Pneumoniae Pneumonia Accompanying High Adenosine Deaminase Activity in Pleural Effusion
- Diagnostic Efficacy of Adenosine Deaminase Isoenzyme in Tuberculous Pleurisy
- Diagnostic Value of Adenosine Deaminase(ADA) and its Isoenzyme in Pleural Effusion
- Diagnostic Significance of TNF-alpha in Tuberculous and Non-Tuberculous Pleural Effusion