Korean J Urol.
2009 Oct;50(10):1027-1031.
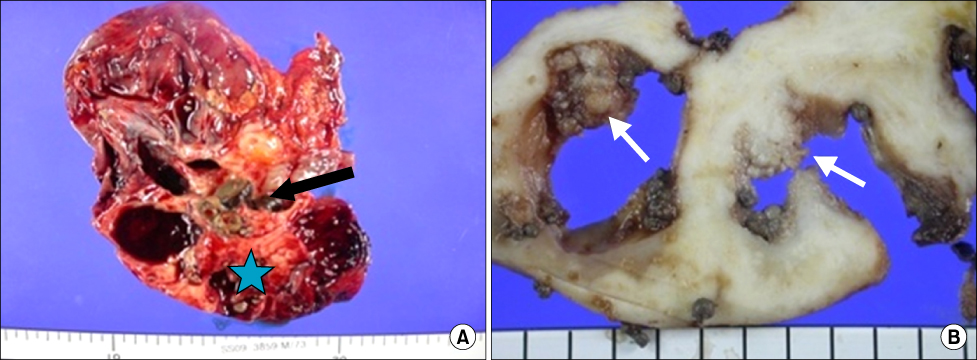
Staghorn Stones Combined with Transitional Cell Carcinoma of the Renal Pelvis
- Affiliations
-
- 1Department of Urology, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. uroman1@yahoo.com
- 2Department of Pathology, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
Abstract
- Longstanding, unrecognized staghorn stones remain a major cause of morbidity in the form of pain, infection, and functional impairment of the affected kidney. Squamous cell carcinoma of the upper urinary tract is associated with stone disease and chronic infection, but the association with transitional cell carcinoma (TCC) has not been proven. We report a case of a 73-year-old man presenting with right flank pain with episodes of total gross hematuria for 1 year. An abdominopelvic computed tomography scan showed decreased parenchymal enhancement and staghorn stones in the right renal pelvis and multiple tiny calyceal stones with severe hydronephrosis. The patient underwent a simple nephrectomy. Histopathologic analysis revealed staghorn stones combined with high-grade papillary TCC of the renal pelvis. The tumor was extended into the peripelvic fat and renal parenchyme (pT3NoMo).
Keyword
MeSH Terms
Figure
Reference
-
1. Kim WJ, Chung JI, Hong JH, Kim CS, Jung SI, Yoon DK. Epidemiological study for urologic cancer in Korea (1998-2002). Korean J Urol. 2004. 45:1081–1088.2. Holmäng S, Lele SM, Johansson SL. Squamous cell carcinoma of the renal pelvis and ureter: incidence, symptoms, treatment and outcome. J Urol. 2007. 178:51–56.3. Preminger GM, Assimos DG, Lingeman JE, Nakada SY, Pearle MS, Wolf JS Jr. Chapter 1: AUA guideline on management of staghorn calculi: diagnosis and treatment recommendations. J Urol. 2005. 173:1991–2000.4. Raghavendran M, Rastogi A, Dubey D, Chaudhary H, Kumar A, Srivastava A, et al. Stones associated renal pelvic malignancies. Indian J Cancer. 2003. 40:108–112.5. Katz R, Gofrit ON, Golijanin D, Landau EH, Shapiro A, Pode D, et al. Urothelial cancer of the renal pelvis in percutaneous nephrolithotomy patients. Urol Int. 2005. 75:17–20.6. Cholankeril JV, Freundlich R, Ketyer S, Spirito AL, Napolitano J. Computed tomography in urothelial tumors of renal pelvis and related filling defects. J Comput Tomogr. 1986. 10:263–272.7. Yeh CC, Lin TH, Wu HC, Chang CH, Chen CC, Chen WC. A high association of upper urinary tract transitional cell carcinoma with nonfunctioning kidney caused by stone disease in Taiwan. Urol Int. 2007. 79:19–23.8. Robert CF. Wein AJ, Kovoussi LR, Novick AC, Partin AW, Peters CA, editors. Urothelial tumors of the upper urinary tract. Campbell-Walsh urology. 2007. 9th ed. Philadelphia: Saunders;1643.9. Hall MC, Womack JS, Roehrborn CG, Carmody T, Sagalowsky AI. Advanced transitional cell carcinoma of the upper urinary tract: patterns of failure, survival and impact of postoperative adjuvant radiotherapy. J Urol. 1998. 160:703–706.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two cases of squamous cell carcinoma with staghorn calculi which were progressed fulminantly
- A Case of Squamous Cell Carcinoma of the Renal Pelvis Associated with Staghorn Calculi
- A case of renal transitional cell carcinoma associated with synchronous contralateral renal cell carcinoma
- Spontaneous Renal Rupture with Renal Pelvis Transitional Cell Carcinoma
- Experience of Transitional Cell Carcinoma after Renal Allograft