Obstet Gynecol Sci.
2015 Nov;58(6):533-536. 10.5468/ogs.2015.58.6.533.
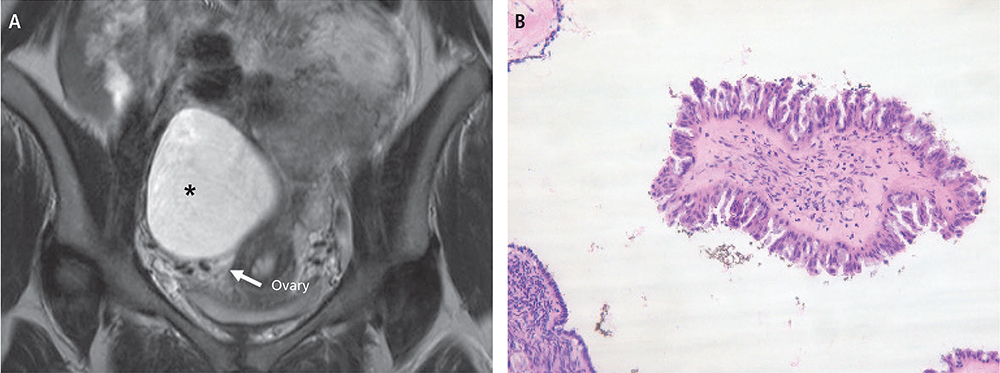
Primary borderline parovarian tumor in pregnancy
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Institute for Medical Sciences, Chonbuk National University Medical School, Jeonju, Korea. obgyn2001@jbnu.ac.kr
- KMID: 2314074
- DOI: http://doi.org/10.5468/ogs.2015.58.6.533
Abstract
- There are few reports of pregnancy complicated by a primary borderline parovarian tumor. A 32-year-old pregnant woman was found to have an ovarian tumor. At 13 weeks of gestation, cystectomy was performed and a diagnosis of primary borderline parovarian tumor was made. At 38 weeks of gestation, she underwent cesarean section combined with a restaging operation. A normal infant was delivered and there were no signs of recurrence. Currently, the patient is being followed for 24 months after the initial treatment and all imaging data show no evidence of recurrence. This report includes a short review of the existing literature on this topic and documents this case in detail. This case demonstrates the appropriate procedure for evaluating and treating a primary borderline parovarian tumor during pregnancy.
Keyword
MeSH Terms
Figure
Reference
-
1. Whitecar MP, Turner S, Higby MK. Adnexal masses in pregnancy: a review of 130 cases undergoing surgical management. Am J Obstet Gynecol. 1999; 181:19–24.2. Jacob JH, Stringer CA. Diagnosis and management of cancer during pregnancy. Semin Perinatol. 1990; 14:79–87.3. Honore LH, O'Hara KE. Serous papillary neoplasms arising in paramesonephric parovarian cysts: a report of eight cases. Acta Obstet Gynecol Scand. 1980; 59:525–528.4. Altaras MM, Jaffe R, Corduba M, Holtzinger M, Bahary C. Primary paraovariancystadenocarcinoma: clinical and management aspects and literature review. Gynecol Oncol. 1990; 38:268–272.5. Seltzer VL, Molho L, Fougner A, Hong P, Kereszti B, Gero M, et al. Parovarian cystadenocarcinoma of low-malignant potential. Gynecol Oncol. 1988; 30:216–221.6. Bider D, Rabinovitch O, Schinder OM, Menczer J. Parovarian serouscystadenocarcinoma of borderline malignancy diagnosed during pregnancy. Gynecol Obstet Invest. 1988; 26:262–264.7. Fine BA, Valente PT, Schroeder B. Parovarian borderline malignancy inpregnancy. Arch Gynecol Obstet. 1996; 258:105–108.8. Fain-Kahn V, Poirot C, Uzan C, Prades M, Gouy S, Genestie C, et al. Feasibility of ovarian cryopreservation in borderline ovarian tumours. Hum Reprod. 2009; 24:850–855.9. Park JY, Kim DY, Kim JH, Kim YM, Kim YT, Nam JH. Surgical management of borderline ovarian tumors: the role of fertility-sparing surgery. Gynecol Oncol. 2009; 113:75–82.10. Kaur K, Gopalan S, Gupta SK, Dhaliwal LK. Parovarian cystadenocarcinoma: a case report. Asia Oceania J Obstet Gynaecol. 1990; 16:131–135.11. Rojansky N, Ophir E, Sharony A, Spira H, Suprun H. Broad ligament adenocarcinoma: its origin and clinical behavior. A literature review and report of a case. Obstet Gynecol Surv. 1985; 40:665–671.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Parovarian Serous Tumor of Borderline Malignancy in Pregnancy
- A case of parovarian tumor of borderline malignancy
- Paraovarian Serous Borderline Tumor: A Case Report
- A case of primary parovarian cystadenocarcinoma of borderline malignancy
- A Case of Parovarian Serous Cystadenocarcinoma of Borderline Malignancy