Obstet Gynecol Sci.
2014 Nov;57(6):560-563. 10.5468/ogs.2014.57.6.560.
Necrotizing ruptured vaginal leiomyoma mimicking a malignant neoplasm
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Gangnam CHA Hospital, CHA University, Seoul, Korea.
- 2Department of Radiology, Gumi CHA Hospital, CHA University, Gumi, Korea.
- 3Department of Pathology, Gumi CHA Hospital, CHA University, Gumi, Korea.
- 4Department of Obstetrics and Gynecology, Gumi CHA Hospital, CHA University, Gumi, Korea. shsong8@gmail.com
- KMID: 2314029
- DOI: http://doi.org/10.5468/ogs.2014.57.6.560
Abstract
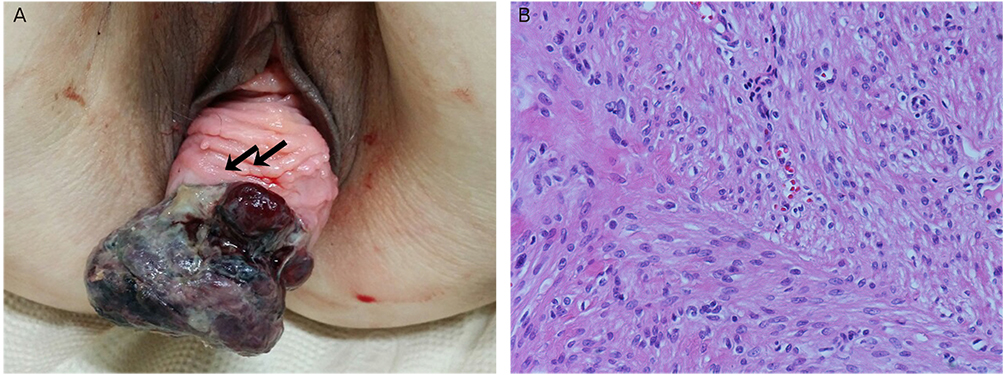
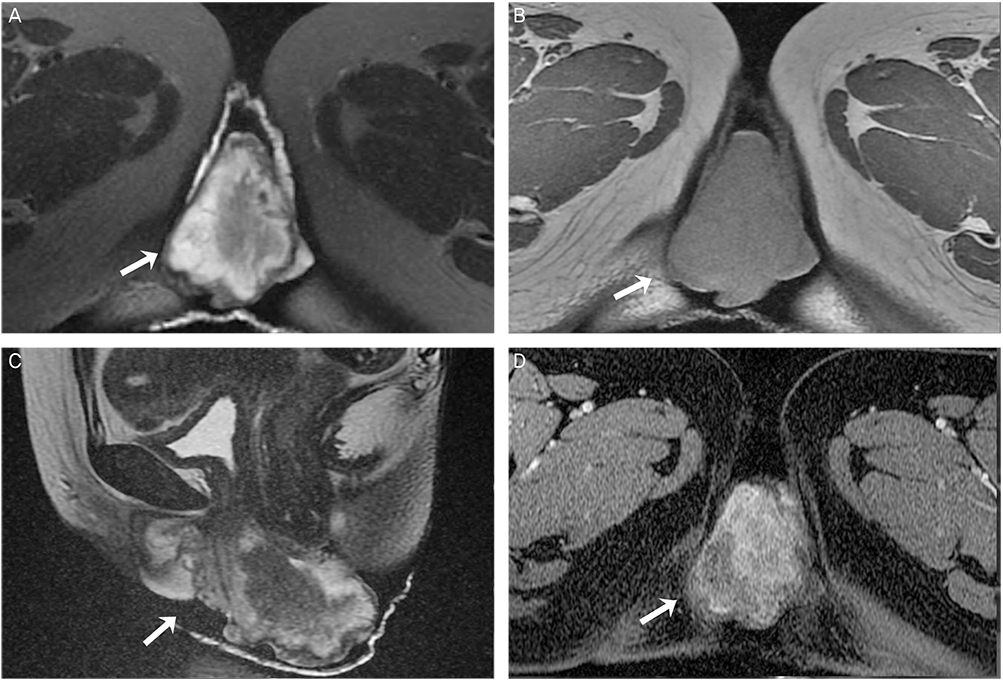
- Leiomyomas are common benign uterine tumors. However, the incidence of vaginal myoma is very rare and may be confused with a variety of vaginal tumors. We report a case of 43-year-old nulligravida who presented with a protruding painful vaginal mass for 7 days. The mass had initially appeared 3 years prior, as 2 to 3 cm that had not subsequently increased. However suddenly, there was rapid severe enlargement over the course of 7 days. Physical exam revealed a monstrous shaped, black color with focal necrosis, odorous protruding vaginal mass about 7 cm in size. The vaginal mass was infected and degenerated. And vaginal wall was also destroyed by the enlarged mass. Because of the clinical features and radiologic findings, the preoperative diagnosis was a vaginal malignancy. We reported an extremely rare case of vaginal myoma that had several characteristics of malignancy, with a brief review of the literature.
Figure
Reference
-
1. Young SB, Rose PG, Reuter KL. Vaginal fibromyomata: two cases with preoperative assessment, resection, and reconstruction. Obstet Gynecol. 1991; 78:972–974.2. Freed SZ, Haleem SA, Wiener I, Feldman J. Bladder outlet obstruction caused by vaginal fibromyoma: the female prostate. J Urol. 1975; 113:30–31.3. Chakrabarti I, De A, Pati S. Vaginal leiomyoma. J Midlife Health. 2011; 2:42–43.4. Bennett HG, Ehrlich MM. Myoma of the vagina. Am J Obstet Gynecol. 1941; 42:314–320.5. Oruc S, Karaer O, Kurtul O. Coexistence of a prolapsed, pedunculated cervical myoma and pregnancy complications: a case report. J Reprod Med. 2004; 49:575–577.6. Liu MM. Fibromyoma of the vagina. Eur J Obstet Gynecol Reprod Biol. 1988; 29:321–328.7. Pavlica P, Bartolone A, Gaudiano C, Barozzi L. Female paraurethral leiomyoma: ultrasonographic and magnetic resonance imaging findings. Acta Radiol. 2004; 45:796–798.8. Shadbolt CL, Coakley FV, Qayyum A, Donat SM. MRI of vaginal leiomyomas. J Comput Assist Tomogr. 2001; 25:355–357.9. Ikeda R, Suga K, Suzuki K. MRI appearance of a leiomyoma of the female urethra. Clin Radiol. 2001; 56:76–79.10. Siegelman ES, Outwater EK. Tissue characterization in the female pelvis by means of MR imaging. Radiology. 1999; 212:5–18.11. Hubert KC, Remer EM, Rackley RR, Goldman HB. Clinical and magnetic resonance imaging characteristics of vaginal and paraurethral leiomyomas: can they be diagnosed before surgery? BJU Int. 2010; 105:1686–1688.12. Cobanoglu O, Gurkan Zorlu C, Ergun Y, Kutluay L. Leiomyosarcoma of the vagina. Eur J Obstet Gynecol Reprod Biol. 1996; 70:205–207.13. Haque AU, Moatasim A, Aslam F. Mitotically active leiomyoma: a word of caution. Int J Pathol. 2004; 2:38–41.14. Ahram J, Lemus R, Schiavello HJ. Leiomyosarcoma of the vagina: case report and literature review. Int J Gynecol Cancer. 2006; 16:884–891.15. Suh DH, Lim SY, Chung J, Choi HJ, Lee S, Park SY. Vaginal leiomyoma mimicking a malignant neoplasm on MR imaging. Korean J Obstet Gynecol. 2006; 49:2432–2437.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vaginal leiomyoma mimicking a malignant neoplasm on MR imaging
- A Case of Suburethral Leiomyoma of the Vagina
- A Case of Leiomyoma of the Vaginal Wall in a Proximal Suburethral and Subtrigonal Location Causing Voiding Difficulty
- A Case of Leiomyoma of the Vagina
- A Case of Leiomyoma of the Uterus and Vagina