Obstet Gynecol Sci.
2013 Sep;56(5):301-306.
A comparative study of methylergonovine and 15-methyl prostaglandin F2alpha in active management of third stage of labor
- Affiliations
-
- 1Department of Pharmacology, MMIMSR, Ambala, India. anshugupta12@hotmail.com
Abstract
OBJECTIVE
Postpartum hemorrhage is most common cause of maternal mortality. Active management of third stage of labor minimizes the risk of postpartum hemorrhage. To compare the effect of methylergonovine and 15-methyl prostaglandin F2alpha (15-methyl PGF2alpha) in active management of third stage of labor.
METHODS
A randomized open labelled parallel study with 50 women in normal labor, 25 in each group were included. The drugs methylergonovine (0.2 mg) intravenous and 15-methyl PGF2alpha (250 microg) intramuscular were administered at the time of delivery of anterior shoulder. Main outcomes measured were amount of blood loss during the first four hours of delivery and objective measurement of hemoglobin and hematocrit levels before delivery and third day postpartum.
RESULTS
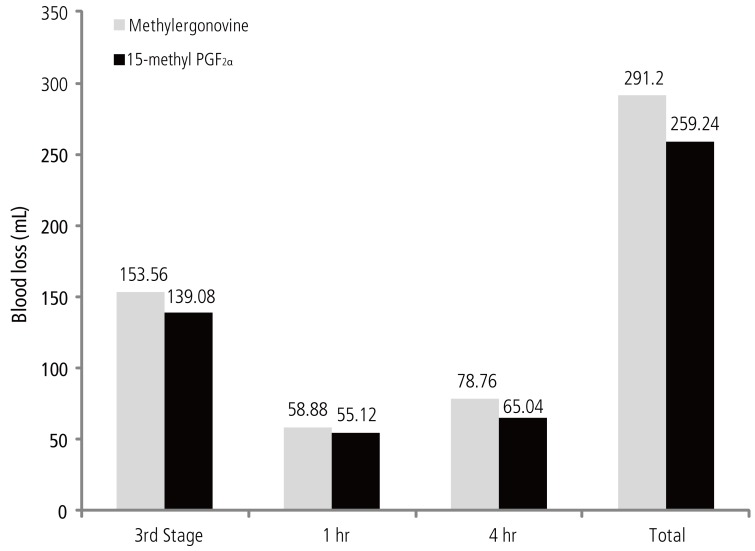
There was no statistically significant difference in the blood loss between the two groups at delivery (P = 0.130), at 1 hour of delivery (P = 0.453). The blood loss with 15-methyl PGF2alpha was significantly less as compared to that of blood loss with methylergonovine at four hours of delivery (P = 0.014) and the total, i.e., during first four hours, amount of blood loss was significantly less with 15-methyl PGF2alpha (P = 0.026). There was no statistically significant difference in the hemoglobin and hematocrit levels measured predelivery and postpartum third day between both the drugs.
CONCLUSION
Both the drugs were effective in controlling the amount of blood loss during the third stage of labor, 15-methyl PGF2alpha being more efficacious.
MeSH Terms
Figure
Reference
-
1. Dildy GA 3rd. Postpartum hemorrhage: new management options. Clin Obstet Gynecol. 2002; 45:330–344. PMID: 12048393.
Article2. El-Refaey H, Nooh R, O'Brien P, Abdalla M, Geary M, Walder J, et al. The misoprostol third stage of labor study: a randomised controlled comparison between orally administered misoprostol and standard management. BJOG. 2000; 107:1104–1110. PMID: 11002953.3. Drife J. Management of primary postpartum haemorrhage. Br J Obstet Gynaecol. 1997; 104:275–277. PMID: 9091001.
Article4. Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Gilstrap LC, Wenstrom KD. Obstetrical hemorrhage. In : Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Gilstrap LC, Wenstrom KD, editors. William's obstetrics. 22nd ed. New York: McGraw-Hill;2005. p. 809–854.5. Bose P, Regan F, Paterson-Brown S. Improving the accuracy of estimated blood loss at obstetric haemorrhage using clinical reconstructions. BJOG. 2006; 113:919–924. PMID: 16907938.
Article6. Sanders-Bush E, Mayer SE. 5-Hydroxytryptamine (serotonin): receptor agonist and antagonist. In : Brunton LL, Lazo JS, Parker KL, editors. Goodman and Gillman's the pharmacological basis of therapeutics. 11th ed. New York: McGraw-Hill;2005. p. 297–315.7. Tripathi KD. 5-Hydroxytryptamine, its antagonists and drug therapy of migraine. In : Tripathi KD, editor. Essential of medical pharmacology. 6th ed. New Delhi: Jaypee brothers;2008. p. 162–172.8. Jaiswal N, Joshi V, Sapre S, Olyai R. Comparative study between per rectal misoprostol and IM methergin for prophylaxis of PPH. Obstet Gynecol Today. 2006; 3:160–162.9. Smyth EM, Burke A, FitzGerald GA. Lipid-derived autacoids: eicosanoids and platelet-activating factor. In : Brunton LL, Lazo JS, Parker KL, editors. Goodman and Gillman's the pharmacological basis of therapeutics. 11th ed. New York: McGraw-Hill;2005. p. 653–670.10. Schuurmans N, MacKinnon C, Lane C, Etches D. Prevention and management of postpartum haemorrhage. SOGC Clinical Practice Guidelines. J Soc Obstet Gynaecol Can. 2000; 22:271–281.11. Schellenberg JC. Primary postpartum haemorrhage (PPH) [Internet]. Versoix, Switzerland: Geneva Foundation for Medical Education and Research;2013. cited 2008 May 24. Available from: http://www.gfmer.ch/Endo/Lectures_09/primary_postpartum_haemorrhage.htm.12. Hofmeyr GJ, Mohlala BK. Hypovolaemic shock. Best Pract Res Clin Obstet Gynaecol. 2001; 15:645–662. PMID: 11478820.
Article13. Gulmezoglu AM, Villar J, Ngoc NT, Piaggio G, Carroli G, Adetoro L, et al. WHO multicentre randomised trial of misoprostol in the management of the third stage of labor. Lancet. 2001; 358:689–695. PMID: 11551574.14. Prendiville WJ, Elbourne D, McDonald S. Active versus expectant management in the third stage of labor. Cochrane Database Syst Rev. 2000; (3):CD000007.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and management of postpartum hemorrhage
- Three Cases of Vitiligo Showing Response to Application of Latanoprost
- The Efficacy and Safety of Inflatable Obstetric Belts for Management of the Second Stage of Labor
- Maternal cardiac arrest after intravenous methylergonovine administration during Cesarean section: A case report
- Prostaglandin E2 for Induction of Labor in Patients with Premature Rupture of Membranes at Term