Obstet Gynecol Sci.
2013 Jul;56(4):265-268.
Prune-belly syndrome detected by ultrasound in the first trimester and the usefulness of vesicocentesis as a modality of treatment
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Chung-Ang University College of Medicine, Seoul, Korea. gjkim@cau.ac.kr
Abstract
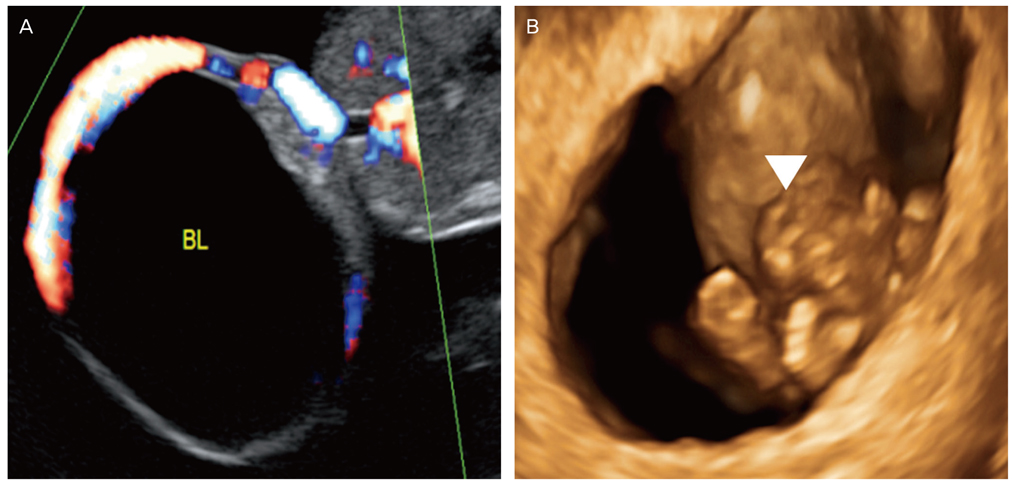
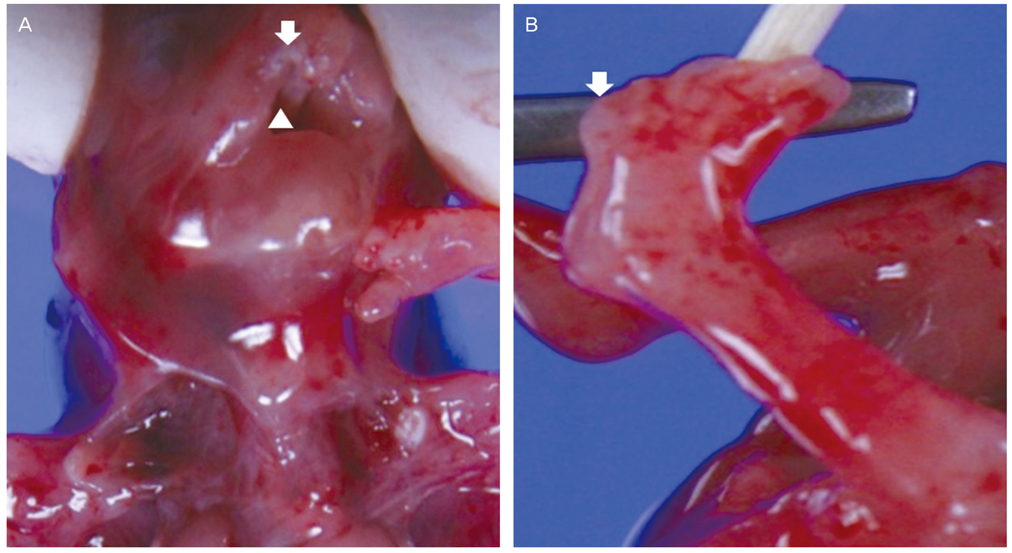
- Prune-belly syndrome may be related to lower urinary tract obstruction (LUTO). LUTO in the early gestational age exacerbates fetal renal function and may require intrauterine intervention. If early developed LUTO causes bladder distension and abdominal musculature deficiency, it will result in prune belly syndrome. Therefore, early detection of the disease and proper treatment before the renal impairment is important. However, there are few literatures concerning the treatment of prune belly syndrome in the first trimester. We report a case of prune belly syndrome diagnosed at 11+6 weeks of gestation and the value of vesicocentesis as a modality of treatment. Ultrasound showed dilated fetal bladder and vesicocentesis was successful in reducing the volume of the bladder. However, the pregnancy was terminated upon request.
Keyword
MeSH Terms
Figure
Reference
-
1. Herman TE, Siegel MJ. Prune belly syndrome. J Perinatol. 2009. 29:69–71.2. Yamamoto H, Nishikawa S, Hayashi T, Sagae S, Kudo R. Antenatal diagnosis of prune belly syndrome at 11 weeks of gestation. J Obstet Gynaecol Res. 2001. 27:37–40.3. Hoshino T, Ihara Y, Shirane H, Ota T. Prenatal diagnosis of prune belly syndrome at 12 weeks of pregnancy: case report and review of the literature. Ultrasound Obstet Gynecol. 1998. 12:362–366.4. Papantoniou N, Papoutsis D, Daskalakis G, Chatzipapas I, Sindos M, Papaspyrou I, et al. Prenatal diagnosis of prune-belly syndrome at 13 weeks of gestation: case report and review of literature. J Matern Fetal Neonatal Med. 2010. 23:1263–1267.5. Hassett S, Smith GH, Holland AJ. Prune belly syndrome. Pediatr Surg Int. 2012. 28:219–228.6. Woodard JR. The prune belly syndrome. Urol Clin North Am. 1978. 5:75–93.7. Crombleholme TM, Harrison MR, Golbus MS, Longaker MT, Langer JC, Callen PW, et al. Fetal intervention in obstructive uropathy: prognostic indicators and efficacy of intervention. Am J Obstet Gynecol. 1990. 162:1239–1244.8. Defoort P, Thiery M. Assessment of the indication for intrauterine treatment of urinary tract malformations. J Perinat Med. 1988. 16:175–181.9. Yiee J, Wilcox D. Abnormalities of the fetal bladder. Semin Fetal Neonatal Med. 2008. 13:164–170.10. Leeners B, Sauer I, Schefels J, Cotarelo CL, Funk A. Prune-belly syndrome: therapeutic options including in utero placement of a vesicoamniotic shunt. J Clin Ultrasound. 2000. 28:500–507.11. Biard JM, Johnson MP, Carr MC, Wilson RD, Hedrick HL, Pavlock C, et al. Long-term outcomes in children treated by prenatal vesicoamniotic shunting for lower urinary tract obstruction. Obstet Gynecol. 2005. 106:503–508.12. Shimada K, Hosokawa S, Tohda A, Matsumoto F, Johnin K. Histology of the fetal prune belly syndrome with reference to the efficacy of prenatal decompression. Int J Urol. 2000. 7:161–166.13. Galati V, Beeson JH, Confer SD, Frimberger D, Campbell JB, Ramji FG, et al. A favorable outcome following 32 vesicocentesis and amnioinfusion procedures in a fetus with severe prune belly syndrome. J Pediatr Urol. 2008. 4:170–172.14. Carroll SG, Soothill PW, Tizard J, Kyle PM. Vesicocentesis at 10-14 weeks of gestation for treatment of fetal megacystis. Ultrasound Obstet Gynecol. 2001. 18:366–370.