Korean J Urol.
2008 Jun;49(6):475-489.
The Present and Future of Prostatitis
- Affiliations
-
- 1Department of Urology, Inje University College of Medicine, Gimhae, Korea. ircho@paik.ac.kr
Abstract
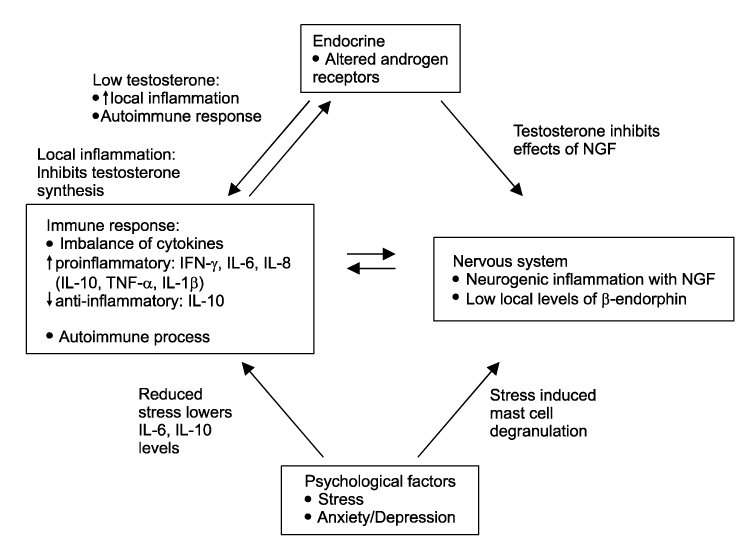
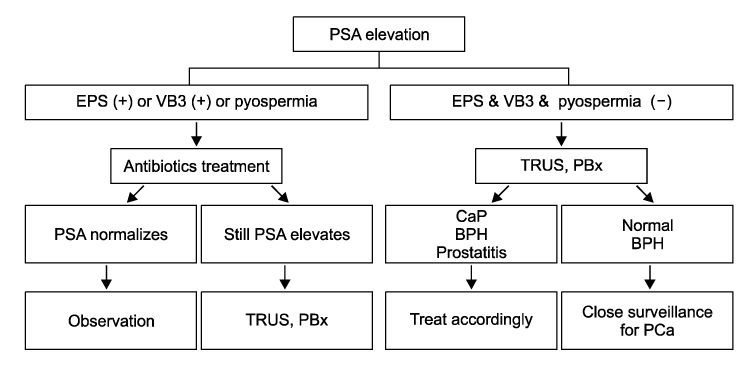
- Prostatitis is a common disease that is confusing and frustrating for urologists. Chronic prostatitis/chronic pelvic pain syndrome(CP/CPPS) is the most common form of prostatitis. The etiology of CP/CPPS is unknown, but possibilities include infectious, autoimmune, neurological, endocrine and psychological causes. Clinical evaluation can aid in diagnosis and follow-up of the patient's response to therapy. Treatment for CP/CPPS is empiric and limited by a lack of randomized, placebo- controlled clinical trials. Antimicrobials are commonly used to treat patients with prostatitis. Other commonly used drugs include alpha-adrenoceptor antagonists, anti-inflammatory drugs, tricyclic antidepressants, and anticholinergic agents. Also, minimally invasive procedures are considered in patients with CP/CPPS and It is possible to treat intractable patients with invasive treatment. Although much progress has been made in therapy, there is no distinct treatment for patients with CP/CPPS. If the concept of neurogenic inflammation with pain is solved, it is possible to treat patients with CP/CPPS at future.
MeSH Terms
Figure
Reference
-
1. Woo YN. Prostatitis. Korean J Urol. 1994. 35:575–585.2. Cho IR. Evaluation and treatment of patients with prostatitis. Korean J Androl. 2005. 23:1–114.3. Fall M, Baranowski AP, Fowler CJ, Lepinard V, Malone-Lee JG, Messelink EJ, et al. EAU guidelines on chronic pelvic pain. Eur Urol. 2004. 46:681–689.4. Wenninger K, Heiman JR, Rothman I, Berghuis JP, Berger RE. Sickness impact of chronic nonbacterial prostatitis and its correlates. J Urol. 1996. 155:965–968.5. Stamey TA. Stamey TA, editor. Urinary tract infections in male. Pathogenesis and treatment of urinary tract infections. 1980. 1st ed. Baltimore: Williams & Wilkins;342–429.6. Nickel JC. Prostatitis: myths and realities. Urology. 1998. 51:362–366.7. Nickel JC, Nigro M, Valiquette L, Anderson P, Patrick A, Mahoney J, et al. Diagnosis and treatment of prostatitis in Canada. Urology. 1998. 52:797–802.8. Meares EM, Stamey TA. Bacteriologic localization patterns in bacterial prostatitis and urethritis. Invest Urol. 1968. 5:492–518.9. Drach GW, Meares EM, Fair WR, Stamey TA. Classification of benign diseases associated with prostatic pain: prostatitis or prostatodynia? J Urol. 1978. 120:266.10. Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999. 282:236–237.11. Krieger JN, Egan KJ, Ross SO, Jacobs R, Berger RE. Chronic pelvic pains represent the most prominent urogenital symptoms of "chronic prostatitis". Urolology. 1996. 48:715–722.12. Goldstraw MA, Fitzpatrick JM, Kirby RS. What is the role of inflammation in the pathogenesis of prostate cancer? BJU Int. 2007. 99:966–968.13. Cho IR, Lee KC, Lee SE, Jeon JS, Park SS, Sung LH, et al. Clinical outcome of acute bacterial prostatitis, a multicenter study. Korean J Urol. 2005. 46:1034–1039.14. Krieger JN, Riley DE. Prostatitis: what is the role of infection. Int J Antimicrob Agents. 2002. 19:475–479.15. Naber KG, Weidner W. Chronic prostatitis - an infectious disease? J Antimicrob Chemother. 2000. 46:157–161.16. Povlsen K, Bjornelius E, Lidbrink P, Lind I. Relationship of Ureaplasma urealyticum biovar 2 to nongonococcal urethritis. Eur J Clin Microbiol Infect Dis. 2002. 21:97–101.17. Pontari MA. Chronic prostatitis/chronic pelvic pain syndrome. Urol Clin North Am. 2008. 35:81–89.18. Pontari MA, Ruggieri MR. Mechanism in prostatitis/chronic pelvic pain syndrome. J Urol. 2004. 172:839–845.19. Hellstrom WJ, Schmidt RA, Lue TF, Tanagho EA. Neuromuscular dysfunction in nonbacterial prostatitis. Urology. 1987. 30:183–188.20. Persson BE, Ronquist G. Evidence for a mechanistic association between nonbacterial prostatitis and levels of urate and creatinine in expressed prostatic secretion. J Urol. 1996. 155:958–960.21. Shoskes DA, Berger R, Elmi A, Landis JR, Propert KJ, Zeitlin S, et al. Muscle tenderness in men with chronic prostatitis/chronic pelvic pain syndrome: the chronic prostatitis cohort study. J Urol. 2008. 179:556–560.22. Alexander RB, Ponniah S, Hasday J, Hebel JR. Elevated levels of proinflammatory cytokines in the semen of patients with chronic prostatitis/chronic pelvic syndrome. Urology. 1998. 52:744–749.23. Berger RE, Miller JE, Rothman I, Krieger JN, Muller CH. Bladder petechiae after cystoscopy and hydrodistension in men daignosed with prostate pain. J Urol. 1998. 159:83–85.24. Nickel JC, Tripp DA, Chuai S, Litwin MS, McNaughton-Collins M, Landis JR, et al. Psychosocial variables affect the quality of life of men diagnosed with chronic prostatitis/chronic pelvic pain syndrome. BJU Int. 2008. 101:59–64.25. Naber KG, Bergman B, Bishop MC, Bierklund Johansen TE, Botto H, Lobel B, et al. EAU Healthcare Office. Guidelines on urinary and male genital tract infections. Guidelines. 2001. 1st ed. Arnhem: EAU;49–56.26. Schaeffer AJ. National Institute of Diabetes and Digestive and Kidney Diseases of the US National Institutes of Health. NIDDK-sponsored chronic prostatitis collaborative research network (CPCRN) 5-year data and treatment guidelines for bacterial prostatitis. Int J Antimicrob Agents. 2004. 24:Suppl 1. S49–S52.27. Roberts RO, Lieber MM, Rhodes T, Girman CJ, Bostwick DG, Jacobsen SJ. Prevalence of a physician-assigned diagnosis of prostatitis: the Olmsted country study of urinary symptoms and health status among men. Urology. 1998. 51:578–584.28. Ku JH, Lee SH, Kim ME, Lee NK, Park YH, Seo YR. Relationship between chronic prostatitis and psychological problem. Korean J Urol. 2001. 42:521–527.29. Kim YS, Choi YD, Kang KH, Ryu RH, Choi HK, Park HS, et al. Study of prostatic disease and symptom between special occupation groups (taxi driver, barber). Korean J Urol. 1998. 39:1093–1097.30. Han MC, Kim JS, Shim BS. Analysis of the risk factors related to progression of chronic prostatitis. Korean J Urol. 2005. 46:1040–1045.31. Bartoletti R, Cai T, Mondaini N, Dinelli N, Pinzi N, Pavone C, et al. Prevalence, incidence estimation, risk factors and characterization of chronic prostatitis/chronic pelvic pain syndrome in urological hospital outpatients in Italy: results of a multicenter case-control observational study. J Urol. 2007. 178:2411–2415.32. Cho IR, Park SC, Park SS. The prevalence of the symptoms of the prostate syndrome patients under 50. Korean J Urol. 1998. 39:751–756.33. Lee JH, Jeon JS, Cho IR. Characteristic symptoms of chronic prostatitis/ chronic pelvic pain syndrome. Korean J Androl. 2002. 43:852–857.34. Yong DJ, Lee SO, Song HD, Oh BS, Cho SY, Jeon JS, et al. Prevalence of premature ejaculation in chronic pelvic pain syndrome. Korean J Androl. 2007. 25:21–25.35. Litwin MS, Collins MM, Fowler FJ Jr, Nickel JC, Calhoun EA, Pontari MA, et al. The national institutes of health chronic prostatitis symptom index: development and validation of a new outcome measure. J Urol. 1999. 162:369–375.36. Shoskes DA, Landis JR, Wang Y, Nickel JC, Zeitlin SI, Nadler R, et al. Impact of post-ejaculatory pain in men with category III chronic prostatitis/chronic pelvic pain syndrome. J Urol. 2004. 172:542–547.37. Roberts RO, Jacobson DJ, Girman CJ, Rhodes T, Lieber MM, Jacobsen SJ. Low agreement between previous physician diagnosed prostatitis and national institutes of health chronic prostatitis symptom index pain measures. J Urol. 2004. 171:279–283.38. Nickel JC. Pre and post massage test (PPMT): a simple screen for prostatitis. Tech Urol. 1997. 3:38–43.39. Ludwig M, Schroeder-Printzen I, Ludecke G, Weidner W. Comparison of expressed prostatic secretions with urine after prostatic massage - a means to diagnose chronic prostatitis/inflammatory chronic pelvic pain syndrome. Urology. 2000. 55:175–177.40. Hennenfent BR, Feliciano AE. Changes in white blood cell counts in men undergoing thrice-weekly prostatic massage, microbial diagnosis and antimicrobial therapy for genitourinary complaints. Br J Urol. 1998. 81:370–376.41. Muller CH, Berger RE, Mohr LE, Krieger JN. Comparison of microscopic methods for detecting inflammation in expressed prostatic secretions. J Urol. 2001. 166:2518–2524.42. Krieger JN, Jacobs R, Ross SO. Detecting urethral and prostatic inflammation in patients with chronic prostatitis. Urology. 2000. 55:186–192.43. McNaughton Collins M, Fowler FJ Jr, Elliott DB, Albertsen PC, Barry MJ. Diagnosis and treating chronic prostatitis: Do urologists use the four-glass test? Urology. 2000. 55:403–407.44. Jang JH, Kim SJ. Anaerobic bacterial isolation in patients with chronic prostatitis syndrome. Korean J Urol. 1994. 35:640–645.45. Berger RE, Krieger JN, Rothman I, Muller CH, Hillier SL. Bacteria in the prostate tissue of men with idiopathic prostatic inflammation. J Urol. 1997. 157:863–865.46. Krieger JN, Riley DE, Roberts MC, Berger RE. Prokaryotic DNA sequences in patients with chronic idiopathic prostatitis. J Clin Microbiol. 1996. 34:3120–3128.47. Krieger JN, Riley DE. Bacteria in the chronic prostatitischronic pelvic pain syndrome: molecular approaches to critical research questions. J Urol. 2002. 167:2574–2583.48. Lee SJ, Cho YH, Kim CS, Shim BS, Cho IR, Chung JI, et al. Screening for Chlamydia and Gonorrhea by strand displacement amplification in homeless adolescents attending youth shelters in Korea. J Korean Med Sci. 2004. 19:495–500.49. Ward BB. How many species of prokaryotes are there? Proc Natl Acad Sci USA. 2002. 99:10234–10236.50. Park SC, Cho IR, Park SS. What are the characteristic transrectal ultrasonographic findings in chronic prostatitis? Korean J Urol. 1998. 39:530–536.51. Patel U, Rickards D. The diagnostic value of colour Doppler flow in the peripheral zone of the prostate, with histological correction. Br J Urol. 1994. 74:590–595.52. Cho IR, Keener TS, Nghiem HV, Winter T, Krieger JN. Prostate blood flow characteristics in the chronic prostatitis/pelvic pain syndrome. J Urol. 2000. 163:1130–1133.53. Kaplan SA, Santarosa RP, D'Alisera PM, Fay BJ, Ikeguchi EF, Hendricks J, et al. Pseudodyssynergia (contraction of the external sphincter during voiding) misdiagnosed as chronic nonbacterial prostatitis and the role of biofeedback as a therapeutic option. J Urol. 1997. 157:2234–2237.54. Lee CU, Seong BM. Urodynamic findings of chronic nonbacterial prostatitis patients with urinary symptoms. Korean J Urol. 2006. 47:268–271.55. Kim TC, Park KH, Kim YK, Lee HS. Endoscopic evaluation ninty-one cases of chronic prostatitis. Korean J Urol. 1962. 3:51–58.56. Cho IR, Kim GJ. Chronic prostatitis and urethritis. Korean J Androl. 1999. 17:33–37.57. Zaichick VY, Sviridova TV, Zaichick SV. Zinc concentration in human prostatic fluid: normal, chronic prostatitis, adenoma and cancer. Int Urol Nephrol. 1996. 28:687–694.58. Nickel JC, Ardern D, Downey J. Cytologic evaluation of urine is important in evaluation of chronic prostatitis. Urology. 2002. 60:225–227.59. Dennis LK, Lynch CF, Torner JC. Epidemiologic association between prostatitis and prostate cancer. Urology. 2002. 60:78–83.60. Roberts RO, Bergstralh EJ, Bass SE, Lieber MM, Jacobsen SJ. Prostatitis as a risk factor for prostate cancer. Epidemiology. 2004. 15:93–99.61. Cho IR, Kim GJ, Park SS, Choi HS. PSA and prostatitis in men under 45 years old. Korean J Urol. 1998. 39:633–637.62. Cho IR, Chang YS, Roh JS, Jeon JS, Park SS. Change of PSA and PSAD after antibiotic treatment in patients with prostatitis. Korean J Androl. 2002. 20:100–105.63. Lee SO, Cho IR, Lee KC, Kim HS. Evaluation of serum prostate specific antigen in subclinical prostatitis: the role of pathology of inflammation. Korean J Urol. 2006. 47:31–36.64. Bozeman CB, Carver BS, Eastham JA, Venable DD. Treatment of chronic prostatitis lowers serum prostate specific antigen. J Urol. 2002. 167:1723–1726.65. Potts JM. Prospective identification of NIH Category IV prostatitis in men with elevated prostate specific antigen. J Urol. 2000. 164:1550–1553.66. Letran JL, Brawer MK. Nicket JC, editor. Prostate specific antigen and prostatitis. Textbook of prostatitis. 1999. 1st ed. Oxford: Isis Medical Media;241–244.67. Dimitrakov JD, Kaplan SA, Kroenke K, Jackson JL, Freeman MR. Management of chronic prostatitis/chronic pelvic pain syndrome: an evidence-based approach. Urology. 2006. 67:881–888.68. Benway BM, Moon TD. Bacterial prostatitis. Urol Clin North Am. 2008. 35:23–32.69. Naber KG, Adam D. Classification of fluoroquinolones. Int J Antimicrobial Agents. 1998. 10:255–257.70. Bjerklund Johansen TE, Gruneberg RN, Guibert J, Hofstetter A, Lobel B, Naber KG, et al. The role of antibiotics in the treatment of chronic prostatitis: a consensus statement. Eur Urol. 1998. 34:457–466.71. Cho IR. Chronic prostatitis/chronic pelvic pain syndrome: guidelines for antibiotic therapy. Korean J UTII. 2006. 1:39–44.72. Lee SD, Lee SJ, Hwang TK, Yoon DK, Lee KS, Sung LH, et al. Multicenter clinical outcome of gatifloxacin for chronic prostatitis (NIH category II or IIIa) in Korea. Korean J UTII. 2007. 2:53–60.73. Baert L, De Ridder D. Weider W, Madsen PO, Schiefer HG, editors. In loco antibiotics in chronic bacterial prostatitis. Prostatitis. 1994. 1st ed. Berlin: Springer-Verlag;191–196.74. Kim YJ, Ryu JK, Lee HJ, Choi WS, Suh JK. Comparison of the efficacy of transperineal intraprostatic injection and oral administration of fluoroquinolone in men with chronic bacterial prostatitis-seminal vesiculitis. Korean J Urol. 2006. 47:1185–1190.75. Kim TH, Kim TH, Kim HR, Lee MK, Myung SC, Kim YS. Detection of cryptic microorganisms in patients with chronic prostatitis by multiplex polymerase chain reaction. Korean J Urol. 2007. 48:304–309.76. Nickel JC, Downey J, Clark J, Casey RW, Pommerville PJ, Barkin J, et al. Levofloxacin for chronic prostatitis/chronic pelvic pain syndrome in men: a randomized placebo-controlled multicenter trial. Urology. 2003. 62:614–617.77. Alexander RB, Propert KJ, Schaeffer AJ, Landis JR, Nickel JC, O'Leary MP, et al. Ciprofloxacin or tamsulosin in men with chronic prostatitis/chronic pelvic pain syndrome: a randomized, double-blind trial. Ann Intern Med. 2004. 141:581–589.78. Jung YH, Kim JG, Cho IR. The efficacy of terazosin in the management of chronic pelvic pain syndrome (CPPS): comparison between category IIIa and IIIb. Korean J Urol. 2006. 47:1191–1196.79. Gul O, Eroglu M, Ozok U. Use of terazosine in patients with chronic pelvic pain syndrome and evaluation by prostatitis symptom score index. Int Urol Nephrol. 2001. 32:433–436.80. Nickel JC, Narayan P, McKay J, Doyle C. Treatment of chronic prostatitis/chronic pelvic pain syndrome with tamsulosin: a randomized double blind trial. J Urol. 2004. 171:1594–1597.81. Mehik A, Alas P, Nickel JC, Sarpola A, Helstrom PJ. Alfuzosin treatment for chronic prostatitis/chronic pelvic pain syndrome: a prospective, randomized, double-blind, placebo-controlled, pilot study. Urology. 2003. 62:425–429.82. Barbalias GA, Nikiforidis G, Liatsikos EN. α-blockers for the treatment of chronic prostatitis in combination with antibiotics. J Urol. 1998. 159:883–887.83. Cheah PY, Liong ML, Yuen KH, Teh CL, Khor T, Yang JR, et al. Initial, long-term, and durable responses to terazosin, placebo, or other therapies for chronic prostatitis/chronic pelvic pain syndrome. Urology. 2004. 64:881–886.84. Geppetti P, Nassini R, Materazzi S, Benemei S. The concept of neurogenic inflammation. BJU Int. 2008. 101(Suppl 3):2–6.85. Trevisani M, Campi B, Gatti R, Andre E, Materazzi S, Nicoletti P, et al. The influence of alpha1-adrenoreceptors on neuropeptide release from primary sensory neurons of the lower urinary tract. Eur Urol. 2007. 52:901–908.86. Shoskes DA, Zeitlin SI, Shahed A, Raifer J. Quercetin in men with category III chronic prostatitis: a preliminary prospective, double-blind, placebo-controlled trial. Urology. 1999. 54:960–963.87. Zermann D, Ishigooka M, Schubert J, Schmidt RA. Perisphincteric injection of botulinum toxin type A. A treatment option for patients with chronic prostatic pain? Eur Urol. 2000. 38:393–399.88. Nickel JC, Downey J, Pontari MA, Shoskes DA, Zeitlin SI. A randomized placebo-controlled multicentre study to evaluate the safety and efficacy of finasteride for male chronic pelvic pain syndrome (category IIIA chronic nonbacterial prostatitis). BJU Int. 2004. 93:991–995.89. Persson BE, Ronquist G, Ekblom M. Ameliorative effect of allopurinol on nonbacterial prostatitis: a parallel double-blind controlled study. J Urol. 1996. 155:961–964.90. Nickel JC, Forrest JB, Tomera K, Hernandez-Graulau J, Moon TD, Schaeffer AJ, et al. Pentosan polysulfate sodium therapy for men with chronic pelvic pain syndrome: a multicenter, randomized, placebo controlled study. J Urol. 2005. 173:1252–1255.91. Shim BS. Complementary and alternative therapy for chronic prostatitis/chronic pelvic pain syndrome. Korean J UTII. 2007. 2:143–150.92. Cornel EB, van Haarst EP, Schaarsberg RW, Geels J. The effect of biofeedback physical therapy in men with chronic pelvic pain syndrome type III. Eur Urol. 2005. 47:607–611.93. Yang SK, Sung WS, Chung H, Kim TW, Kim HS, Lho YS. Biofeedback and functional electrical stimulation therapy for patients with intractable chronic pelvic pain syndrome. Korean J Urol. 2003. 44:1220–1224.94. Lee KC, Choi H, Park HS, Kim JJ, Moon DG. Therapeutic efficacy of extracorporeal magnetic therapy in chronic pelvic pain syndrome. Korean J Urol. 2003. 44:693–696.95. Kim SW, Kim SH, Lee CH, Lee SJ, Cho YH, Yoon MS. Clinical efficacy of extracorporeal magnetic innervation for chronic pelvic pain syndrome. Korean J Androl. 2003. 21:44–47.96. Yavascaoglu I, Oktay B, Simşek U, Ozyurt M. Role of ejaculation in the treatment of chronic non-bacterial prostatitis. Int J Urol. 1999. 6:130–134.97. Kastner C, Hochreiter W, Huidobro C, Cabezas J, Miller P. Cooled transurethral microwave thermotherapy for intractable chronic prostatitis - results of a pilot study after 1 year. Urology. 2004. 64:1149–1154.98. Leskinen MJ, Kilponen A, Lukkarinen O, Tammela TL. Transurethral needle ablation for the treatment of chronic pelvic pain syndrome (category III prostatitis): a randomized, sham-controlled study. Urology. 2002. 60:300–304.99. Desireddi NV, Campbell PL, Stern JA, Sobkoviak R, Chuai S, Shahrara S, et al. Monocyte chemoattractant protein-1α and macrophage inflammatory protein-1a as possible biomarkers for the chronic pelvic pain syndrome. J Urol. 2008. 179:1857–1862.