Korean J Urol.
2008 Aug;49(8):739-744.
The Clinical Experience of Genital Pelvic OrganProlapse with the Prolift(TM) System
- Affiliations
-
- 1Department of Urology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. mschoo@amc.seoul.kr
- 2Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
Abstract
-
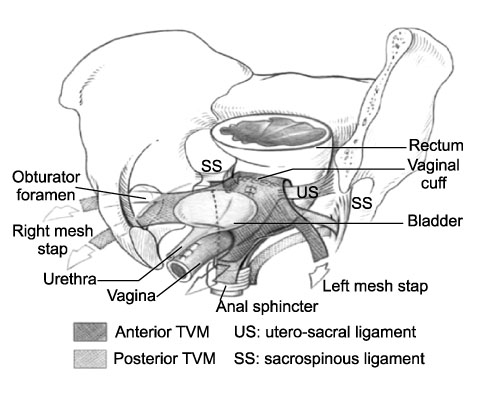
PURPOSE: In the surgical treatment of pelvic organ prolapse(POP), treatment failure and re-operation rates are relatively high when conventional mesh-free surgical methods are employed. Recently, a transvaginal prolapse repair method using surgical mesh has come into broad usage. The principal objective of this study was to report on the clinical efficacy and safety of transvaginal mesh repair of genital prolapses using the Prolift(TM) system.
MATERIALS AND METHODS
We included 31(mean age 61.1 years) patients who had undergone pelvic organ prolapsed treatment with the Prolift(TM) system. The evaluation included a medical history, physical examination including Pelvic Organ Prolapse staging system(POP-Q), a urodynamic study, and a Pelvic Floor Distress Inventory(PFDI). An anatomic cure after intervention was defined as stage 0 and an improvement was defined as stage I. Anatomic failures were defined as stage II or higher. The patients were monitored at 4, 12 and 52 weeks postoperatively, and the mean follow-up period was 13.7 months.
RESULTS
Preoperative anterior vaginal wall prolapse to the POP-Q was stage II in 13, III in 14, IV in 4, uterine or vaginal vault prolapse stage II in 3, III in 6, IV in 1 and posterior vaginal wall prolapse stage II in 3, and stage III in 7. Anterior, posterior and total repair were performed in 21(67.8%), 1(3.2%), and 9(29.0%) patients, respectively. 90.3%(28/31) of the patients had been anatomically cured upon follow-up examination, and 93.5%(29/31) reported being satisfied with the result of the operation. Pre-and postoperative urinary symptoms, as well as prolapse symptoms as evaluated by PFDI, were improved significantly.
CONCLUSIONS
Pelvic floor surgery using the Prolift(TM) system appears to be both effective and safe.
Keyword
MeSH Terms
Figure
Reference
-
1. Beck RP, McCormick S, Nordstrom L. A 25-year experience with 519 anterior colporrhaphy procedures. Obstet Gynecol. 1991. 78:1011–1018.2. Porges RF, Smilen SW. Long-term analysis of the surgical management of pelvic support defects. Am J Obstet Gynecol. 1994. 171:1518–1526.3. Clark AL, Gregory T, Smith VJ, Edwards R. Epidemiologic evaluation of reoperation for surgically treated pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol. 2003. 189:1261–1267.4. Whiteside JL, Weber AM, Meyn LA, Walters MD. Risk factors for prolapse recurrence after vaginal repair. Am J Obstet Gynecol. 2004. 191:1533–1538.5. Iglesia CB, Fenner DE, Brubaker L. The use of mesh in gynecologic surgery. Int Urogynecol J Pelvic Floor Dysfunct. 1997. 8:105–115.6. Fatton B, Amblard J, Debodinance P, Cosson M, Jacquetin B. Transvaginal repair of genital prolapse: preliminary results of a new tension-free vaginal mesh (prolift™ technique): a case series multicentric study. Int Urogynecol J Pelvic Floor Dysfunct. 2007. 18:743–752.7. Altman D, Vayrynen T, Engh ME, Axelsen S, Falconer C. Short-term outcome after transvaginal mesh repair of pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2007. [Epub ahead of print].8. Collinet P, Belot F, Debodinance P, Ha Duc E, Lucot JP, Cosson M. Transvaginal mesh technique for pelvic organ prolapse repair: mesh exposure management and risk factors. Int Urogynecol J Pelvic Floor Dysfunct. 2006. 17:315–320.9. Weber AM, Abrams P, Brubaker L, Cundiff G, Davis G, Dmochowski RR, et al. The standardization of terminology for researchers in female pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct. 2001. 12:178–186.10. Milani R, Salvatore S, Soligo M, Pifarotti P, Meschia M, Cortese M. Functional and anatomical outcome of anterior and posterior vaginal prolapse repair with prolene mesh. BJOG. 2005. 112:107–111.11. Reisenauer C, Kirschniak A, Drews U, Wallwiener D. Anatomical conditions for pelvic reconstruction with polyprolylene implant and its application for the treatment of vaginal prolapse. Eur J Obstet Gynecol. 2007. 131:214–225.12. Choi YS, Choo MS, Lee KS. Efficacy and safety of cystocele repair reinforced with a monofilament polypropylene mesh. Korean J Urol. 2006. 47:640–644.13. Deffieux X, de Tayrac R, Huel C, Bottero J, Gervaise A, Bonnet K, et al. Vaginal mesh erosion after transvaginal repair of cystocele using Gynemesh or Gynemesh-Soft in 138 women: a comparative study. Int Urogynecol J Pelvic Floor Dysfunct. 2007. 18:73–79.14. de Tayrac R, Picone O, Chauveaud-Lambling A, Fernandez H. A 2-year anatomical and functional assessment of transvaginal rectocele repair using a polypropylene mesh. Int Urogynecol J Pelvic Floor Dysfunct. 2006. 17:100–105.15. Cosson M, Caquant F, Collinet P, Rosenthal C, Clave H, Debodinance P, editors. Prolift (mesh Gynecare) for pelvic organ prolapse surgical treatment using the TVM group technique: a retrospective study of 687 patients. Communication in the ICS meeting. 2005. Montreal.16. Baessler K, Maher CF. Mesh augmentation during pelvic-floor reconstructive surgery: risks and benefits. Curr Opin Obstet Gynecol. 2006. 18:560–566.17. Brun JL, Bordenave L, Lefedvre F, Bareille R, Barbie C, Rouais F, et al. Physical and biological characteristics of the main biomaterials used in pelvic surgery. Biomed Mater Eng. 1992. 2:203–225.18. Jo HI, Kim JW, Park NH, Kang SB, Lee HP, Song YS. Efficacy and outcome of anterior vaginal wall repair using polypropylene mesh (Gynemesh). J Obstet Gynecol. 2007. 33:700–704.19. McGuire EJ, Gardy M, Elkins T, DeLancey JO. Treatment of incontinence with pelvic prolapse. Urol Clin North Am. 1991. 18:349–353.20. Rosenzweing BA, Pushkin S, Blumenfeld D, Bhatia NN. Prevalence of abnormal urodynamic test result in continent women with severe genitourinary prolapse. Obstet Gynecol. 1992. 79:539–542.21. Sentilhes L, Berthier A, Sergent F, Verspyck E, Descamps P, Marpeau L. Sexual function in women before and after transvaginal mesh repair for pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2007. [Epub ahead of print].
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Initial Experience with Concomitant Prolift(TM) System and Tension-Free Vaginal Tape Procedures in Patients with Stress Urinary Incontinence and Cystocele
- A Case of Genital Prolapse in Premature Baby
- First Experience of Cardiac Surgery using da Vinci(TM) Surgical System in Korea
- First Experience of Thoracic Surgery with the da Vinci(TM) Surgical System in Korea
- Clinical Experience of the Reverse Iontophoresis Based Glucose Measuring System: Glucall(TM)