J Cardiovasc Ultrasound.
2016 Jun;24(2):115-122. 10.4250/jcu.2016.24.2.115.
The Combined Impact of Neutrophil-to-Lymphocyte Ratio and Type 2 Diabetic Mellitus on Significant Coronary Artery Disease and Carotid Artery Atherosclerosis
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Convergence Medicine & Exercise Science Research Institute, Kosin University School of Medicine, Busan, Korea. kyoungim74@gmail.com
- 2Department of Statistics and Actuarial Science, Soongsil University, Seoul, Korea.
- KMID: 2308700
- DOI: http://doi.org/10.4250/jcu.2016.24.2.115
Abstract
- BACKGROUND
Neutrophil-to-lymphocyte ratio (NLR) has recently emerged as a new important inflammatory marker for predicting cardiovascular events. This study aimed to evaluate the combined impact of NLR and type 2 diabetes mellitus (T2DM) on significant coronary artery disease (CAD) and carotid artery atherosclerosis.
METHODS
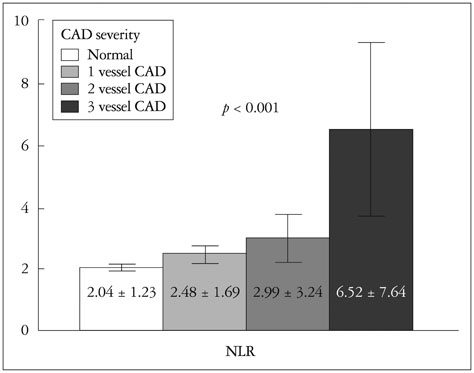
This study includes a total of 828 patients evaluated by coronary angiography and carotid ultrasonography. Significant CAD was defined as at least one vessel with stenosis greater than 50%. We employed logistic regression models to investigate the association of NLR and T2DM with significant CAD. The goodness-of-fit and discriminability of the models were assessed by the loglikelihood ratio test and C-index, respectively. Also, we investigated the clinical relevance of the categorized NLR that classifies patients into three risk groups (low, intermediate, high).
RESULTS
According to logistic regression analysis, both NLR {adjusted odds ratio (OR) 1.31, p < 0.001} and T2DM (adjusted OR 2.46, p = 0.006) were independent risk factors of significant CAD. The addition of NLR and T2DM into a logistic regression model including conventional cardiovascular risk factors significantly improved the goodness-of-fit (p < 0.001) and the discriminability of the model (p = 0.004). Also, T2DM patients assigned into the high risk group (NLR > 2) showed the greater prevalence of significant CAD and carotid artery atherosclerosis compared with patients without T2DM or type 2 diabetic patients assigned into the low risk group (NLR ≤ 1).
CONCLUSION
Our results suggest that type 2 diabetic patients with high inflammatory state would be more vulnerable to significant CAD and carotid artery atherosclerosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Ross R. Atherosclerosis--an inflammatory disease. N Engl J Med. 1999; 340:115–126.2. Libby P. What have we learned about the biology of atherosclerosis? The role of inflammation. Am J Cardiol. 2001; 88(7B):3J–6J.3. Lee GK, Lee LC, Chong E, Lee CH, Teo SG, Chia BL, Poh KK. The long-term predictive value of the neutrophil-to-lymphocyte ratio in type 2 diabetic patients presenting with acute myocardial infarction. QJM. 2012; 105:1075–1082.4. Lou M, Luo P, Tang R, Peng Y, Yu S, Huang W, He L. Relationship between neutrophil-lymphocyte ratio and insulin resistance in newly diagnosed type 2 diabetes mellitus patients. BMC Endocr Disord. 2015; 15:9.5. Kaya H, Ertaç F, Soydinç MS. Association between neutrophil to lymphocyte ratio and severity of coronary artery disease. Clin Appl Thromb Hemost. 2014; 20:221.6. Acet H, Ertaş F, Akıl MA, Oylumlu M, Polat N, Yıldız A, Bilik MZ, Yüksel M, Kaya Z, Ulgen MS. New inflammatory predictors for nonvalvular atrial fibrillation: echocardiographic epicardial fat thickness and neutrophil to lymphocyte ratio. Int J Cardiovasc Imaging. 2014; 30:81–89.7. Park BJ, Shim JY, Lee HR, Lee JH, Jung DH, Kim HB, Na HY, Lee YJ. Relationship of neutrophil-lymphocyte ratio with arterial stiffness and coronary calcium score. Clin Chim Acta. 2011; 412:925–929.8. Kim JA, Choi CJ, Yum KS. Cut-off values of visceral fat area and waist circumference: diagnostic criteria for abdominal obesity in a Korean population. J Korean Med Sci. 2006; 21:1048–1053.9. Vermeersch SJ, Rietzschel ER, De Buyzere ML, Van Bortel LM, D’Asseler Y, Gillebert TC, Verdonck PR, Segers P. Validation of a new automated IMT measurement algorithm. J Hum Hypertens. 2007; 21:976–978.10. Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, Csiba L, Desvarieux M, Ebrahim S, Hernandez Hernandez R, Jaff M, Kownator S, Naqvi T, Prati P, Rundek T, Sitzer M, Schminke U, Tardif JC, Taylor A, Vicaut E, Woo KS. Mannheim carotid intimamedia thickness and plaque consensus (2004-2006-2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovasc Dis. 2012; 34:290–296.11. Choi JO, Shin MS, Kim MJ, Jung HO, Park JR, Sohn IS, Kim H, Park SM, Yoo NJ, Choi JH, Kim HK, Cho GY, Lee MR, Park JS, Shim CY, Kim DH, Shin DH, Shin GJ, Shin SH, Kim KH, Park JH, Lee SY, Kim WS, Park SW. Normal echocardiographic measurements in a Korean population study: part I. Cardiac chamber and great artery evaluation. J Cardiovasc Ultrasound. 2015; 23:158–172.12. Kim HS, Cho KI. Association of carotid artery parameters of atherosclerosis in coronary artery disease. J Cardiovasc Ultrasound. 2013; 21:72–80.13. Gnasso A, Carallo C, Irace C, Spagnuolo V, De Novara G, Mattioli PL, Pujia A. Association between intima-media thickness and wall shear stress in common carotid arteries in healthy male subjects. Circulation. 1996; 94:3257–3262.14. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a non-parametric approach. Biometrics. 1988; 44:837–845.15. Vinh-Hung V, Verkooijen HM, Fioretta G, Neyroud-Caspar I, Rapiti E, Vlastos G, Deglise C, Usel M, Lutz JM, Bouchardy C. Lymph node ratio as an alternative to pN staging in node-positive breast cancer. J Clin Oncol. 2009; 27:1062–1068.16. Pitsavos C, Tampourlou M, Panagiotakos DB, Skoumas Y, Chrysohoou C, Nomikos T, Stefanadis C. Association between low-grade systemic inflammation and type 2 diabetes mellitus among men and women from the ATTICA study. Rev Diabet Stud. 2007; 4:98–104.17. Dalla Vestra M, Mussap M, Gallina P, Bruseghin M, Cernigoi AM, Saller A, Plebani M, Fioretto P. Acute-phase markers of inflammation and glomerular structure in patients with type 2 diabetes. J Am Soc Nephrol. 2005; 16:Suppl 1. S78–S82.18. Shoelson SE, Lee J, Goldfine AB. Inflammation and insulin resistance. J Clin Invest. 2006; 116:1793–1801.19. Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, Sole J, Nichols A, Ross JS, Tartaglia LA, Chen H. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest. 2003; 112:1821–1830.20. Rajwani A, Cubbon RM, Wheatcroft SB. Cell-specific insulin resistance: implications for atherosclerosis. Diabetes Metab Res Rev. 2012; 28:627–634.21. Sunbul M, Gerin F, Durmus E, Kivrak T, Sari I, Tigen K, Cincin A. Neutrophil to lymphocyte and platelet to lymphocyte ratio in patients with dipper versus non-dipper hypertension. Clin Exp Hypertens. 2014; 36:217–221.22. Okyay GU, Inal S, Oneç K, Er RE, Paoşaoğlu O, Paoşaoğlu H, Derici U, Erten Y. Neutrophil to lymphocyte ratio in evaluation of inflammation in patients with chronic kidney disease. Ren Fail. 2013; 35:29–36.23. Tamhane UU, Aneja S, Montgomery D, Rogers EK, Eagle KA, Gurm HS. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am J Cardiol. 2008; 102:653–657.24. Cho KI, Ann SH, Singh GB, Her AY, Shin ES. Combined usefulness of the platelet-to-lymphocyte ratio and the neutrophil-to-lymphocyte ratio in predicting the long-term adverse events in patients who have undergone percutaneous coronary intervention with a drug-eluting stent. PLoS One. 2015; 10:e0133934.25. Verdoia M, Schaffer A, Barbieri L, Aimaretti G, Marino P, Sinigaglia F, Suryapranata H, De Luca G; Novara Atherosclerosis Study Group (NAS). Impact of diabetes on neutrophil-to-lymphocyte ratio and its relationship to coronary artery disease. Diabetes Metab. 2015; 41:304–311.26. O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK Jr. Cardiovascular Health Study Collaborative Research Group. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. N Engl J Med. 1999; 340:14–22.27. Chambless LE, Heiss G, Folsom AR, Rosamond W, Szklo M, Sharrett AR, Clegg LX. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987-1993. Am J Epidemiol. 1997; 146:483–494.28. Naqvi TZ, Lee MS. Carotid intima-media thickness and plaque in cardiovascular risk assessment. JACC Cardiovasc Imaging. 2014; 7:1025–1038.29. Asakura T, Karino T. Flow patterns and spatial distribution of atherosclerotic lesions in human coronary arteries. Circ Res. 1990; 66:1045–1066.30. Thomson SP, McMahon LJ, Nugent CA. Endogenous cortisol: a regulator of the number of lymphocytes in peripheral blood. Clin Immunol Immunopathol. 1980; 17:506–514.31. Naruko T, Ueda M, Haze K, van der Wal AC, van der Loos CM, Itoh A, Komatsu R, Ikura Y, Ogami M, Shimada Y, Ehara S, Yoshiyama M, Takeuchi K, Yoshikawa J, Becker AE. Neutrophil infiltration of culprit lesions in acute coronary syndromes. Circulation. 2002; 106:2894–2900.32. Chapman CM, Beilby JP, McQuillan BM, Thompson PL, Hung J. Monocyte count, but not C-reactive protein or interleukin-6, is an independent risk marker for subclinical carotid atherosclerosis. Stroke. 2004; 35:1619–1624.33. Raitakari M, Mansikkaniemi K, Marniemi J, Viikari JS, Raitakari OT. Distribution and determinants of serum high-sensitive C-reactive protein in a population of young adults: The Cardiovascular Risk in Young Finns Study. J Intern Med. 2005; 258:428–434.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neutrophil-to-Lymphocyte Ratio for Risk Assessment in Coronary Artery Disease and Carotid Artery Atherosclerosis
- Carotid ultrasound in patients with coronary artery disease
- Association of carotid atherosclerosis and obesity in type 2 diabetic patients
- Relationship Between Carotid and Coronary Atherosclerosis in the Elderly
- Correlation between Intima-Media Thickness in Carotid Artery and the Extent of Coronary Atherosclerosis