J Korean Orthop Assoc.
2016 Jun;51(3):214-220. 10.4055/jkoa.2016.51.3.214.
Comparative Analysis of Revision Surgery Groups between within 5 Years and More than 10 Years after Lumbar Spinal Fusion Due to Adjacent Segment Disease
- Affiliations
-
- 1Department of Orthopedic Surgery, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea.
- 2Department of Orthopedic Surgery and Spine Center, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea. schsbj@schmc.ac.kr
- KMID: 2308582
- DOI: http://doi.org/10.4055/jkoa.2016.51.3.214
Abstract
- PURPOSE
The purpose of this study is to analyze the risk factors for early adjacent segment disease (EASD) in patients undergoing revision surgery within 5 years from the first operation as compared with those after more than 10 years.
MATERIALS AND METHODS
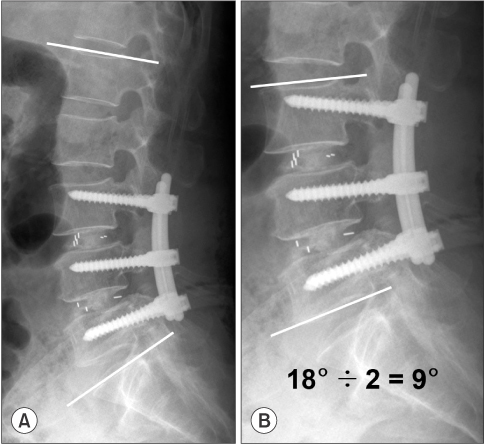
A total of 755 patients with degenerative lumbar disease underwent lumbar spinal fusion of 3 or less segments between August, 1988 and May, 2009. Of these, 44 patients underwent revision surgery due to adjacent segment disease (ASD) until May, 2014. These patients presented with ASD, 19 and 13 of whom underwent revision surgery within 5 years and after more than 10 years of the first one, and were thus assigned to group A (n=19) and group B (n=13), respectively. Thirty-two of these patients were enrolled in this study and baseline and clinical characteristics, including sex, age, fusion method, preoperative diagnosis, the number of fused segments, fusion level, and radiological measurements were compared between the two groups. Radiological measurements included pre- and postoperative lumbar lordotic angle (LLA), pre- and postoperative fusion segment lordotic angle (FSLA), pre- and postoperative FSLA per level and the correction of LLA, FSLA, and FSLA per level. For statistical analysis, univariate analysis with the chi-square test was performed using SPSS 14.0.
RESULTS
In group A, the number of patients undergoing posterior lumbar interbody fusion (PLIF) rather than posterolateral fusion, those with postoperative FSLA per level of <20° and the adjacent segment levels to L4-5 and L5-S1 was significantly larger compared with group B (p=0.018, 0.046, and 0.009, respectively.
CONCLUSION
In conclusion, our results indicate that the degree of risk of EASD was relatively higher in association with PLIF, postoperative FSLA per level of <20° and the adjacent segment levels to L4-5 and L5-S1.
Figure
Reference
-
1. Kim HT, Kang DW, Yoo CH, Jeoung JH, Chang SA. Late changes at the adjacent segments to lumbar fusions. J Korean Soc Spine Surg. 1996; 3:1–10.2. Ahn DK, Lee S, Jeong KW, Park JS, Cha SK, Park HS. Adjacent segment failure after lumbar spine fusion: controlled study for risk factors. J Korean Orthop Assoc. 2005; 40:203–208.
Article3. Kim HT, Park BH, Cheon DW, Kim HP, Jeoung JH. The changes of angular motion in the adjacent segments to lumbar fusions. J Korean Soc Spine Surg. 1995; 2:1–10.4. Kumar MN, Jacquot F, Hall H. Long-term follow-up of functional outcomes and radiographic changes at adjacent levels following lumbar spine fusion for degenerative disc disease. Eur Spine J. 2001; 10:309–313.
Article5. Ha KY, Kim YH, Kang KS. Surgery for adjacent segment changes after lumbosacral fusion. J Korean Soc Spine Surg. 2002; 9:332–340.
Article6. Etebar S, Cahill DW. Risk factors for adjacent-segment failure following lumbar fixation with rigid instrumentation for degenerative instability. J Neurosurg. 1999; 90:2 Suppl. 163–169.
Article7. Aota Y, Kumano K, Hirabayashi S. Postfusion instability at the adjacent segments after rigid pedicle screw fixation for degenerative lumbar spinal disorders. J Spinal Disord. 1995; 8:464–473.
Article8. Lee JC, Kim Y, Soh JW, Shin BJ. Risk factors of adjacent segment disease requiring surgery after lumbar spinal fusion: comparison of posterior lumbar interbody fusion and posterolateral fusion. Spine (Phila Pa 1976). 2014; 39:E339–E345.9. Lee KY, Sohn SK, Lee MJ, Wang L. Risk Factors for Adjacent Segment Disease after Posterolateral Lumbar Fusion. J Korean Soc Spine Surg. 2008; 15:174–182.
Article10. Brodsky AE. Post-laminectomy and post-fusion stenosis of the lumbar spine. Clin Orthop Relat Res. 1976; (115):130–139.
Article11. Stokes IA, Wilder DG, Frymoyer JW, Pope MH. 1980 Volvo award in clinical sciences. Assessment of patients with low-back pain by biplanar radiographic measurement of intervertebral motion. Spine (Phila Pa 1976). 1981; 6:233–240.12. Frymoyer JW, Hanley EN Jr, Howe J, Kuhlmann D, Matteri RE. A comparison of radiographic findings in fusion and nonfusion patients ten or more years following lumbar disc surgery. Spine (Phila Pa 1976). 1979; 4:435–440.
Article13. Goel VK, Weinstein JN, Liu YK, Kim YE, Okuma T. Biomechanics of spine stabilization. In : Weinstein JN, Wiesel SW, editors. The lumbar spine. Philadelphia: WB Saunders Co;1990. p. 195–212.14. Brodsky AE, Hendricks RL, Khalil MA, Darden BV, Brotzman TT. Segmental ("floating") lumbar spine fusions. Spine (Phila Pa 1976). 1989; 14:447–450.
Article15. Dekutoski MB, Schendel MJ, Ogilvie JW, Olsewski JM, Wallace LJ, Lewis JL. Comparison of in vivo and in vitro adjacent segment motion after lumbar fusion. Spine (Phila Pa 1976). 1994; 19:1745–1751.
Article16. Grouw AV, Nadel CI, Weierman RJ, Lowell HA. Long term follow-up of patients with idiopathic scoliosis treated surgically: a preliminary subjective study. Clin Orthop Relat Res. 1976; 117:197–201.
Article17. Chung JY, Seo HY, Jung JW. Surgical treatment of adjacent degenerative segment after lumbar fusion: preliminary report. J Korean Soc Spine Surg. 2000; 7:264–270.18. Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. 1991; 73:802–808.
Article19. Cho JL, Park YS, Han JH, Lee CH, Roh WI. The changes of adjacent segments after spinal fusion: follow-up more than three years after spinal fusion. J Korean Soc Spine Surg. 1998; 5:239–246.20. Ahn DK, Lee S, Jeong KW, Choi DJ, Cha SK, Cho KH. Degenerative change of adjacent segments according to the fusion method after l4-5 segmental fusion: comparative study of posterolateral fusion and posterior lumbar interbody fusion. J Korean Orthop Assoc. 2006; 41:281–287.
Article21. Soh J, Lee JC, Shin BJ. Analysis of risk factors for adjacent segment degeneration occurring more than 5 years after fusion with pedicle screw fixation for degenerative lumbar spine. Asian Spine J. 2013; 7:273–281.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Revision Surgery for Spinal Stenosis Developed at the Adjacent Segment after Lumbar Fusion
- Biportal Endoscopic Transforaminal Interbody Fusion for Lumbar Adjacent Segment Disease: An Illustrative Case and Literature Review
- Revision Arthrodesis After Lumbar Fusion in Degenerative Lumbar Disease
- The Revision Operation Rate for Adjacent Segmental Degeneration by Survival Analysis in Mono-segment Lumbar Fusion
- A Comparison of Adjacent Segment Diseases Above One Versus Above Two Vertebral Segment after Spinal Fusion of the Degenerative Lumbar Disease