J Korean Orthop Assoc.
2016 Jun;51(3):199-206. 10.4055/jkoa.2016.51.3.199.
Risk Factors of Cervical Spondylosis in Workers Requiring Neck Flexion and Extension Actions in Farming and Fishing Communities
- Affiliations
-
- 1Department of Orthopaedic Surgery, Gyeongsang National University School of Medicine, Jinju, Korea. dhkim8311@gnu.ac.kr
- 2Department of Preventive Medicine, Gyeongsang National University School of Medicine, Jinju, Korea.
- 3Center for Farmer's Safety and Health, Gyeongsang National University Hospital, Jinju, Korea.
- KMID: 2308580
- DOI: http://doi.org/10.4055/jkoa.2016.51.3.199
Abstract
- PURPOSE
The purpose of this study is to determine the relationship between the repetitive flexion or extension posture on the cervical spine on labor and degenerative change of the cervical spine, and the factors affecting degenerative change of the cervical spine.
MATERIALS AND METHODS
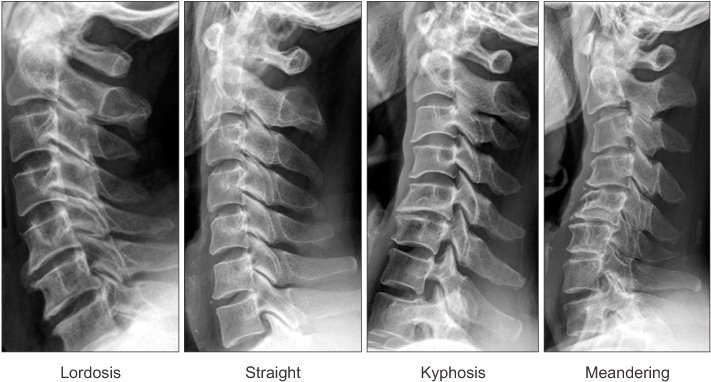
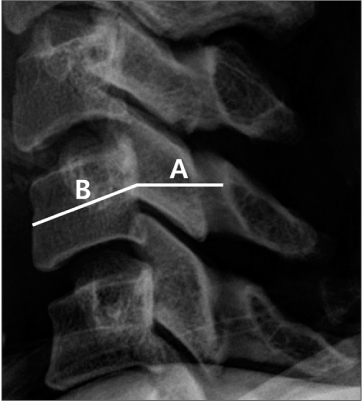
To determine the factors affecting degenerative change of the cervical spine, age, sex, height, weight, body mass index, smoking, diabetes mellitus (DM), time engaging in labor, and cervical spine posture (flexion or extension) required repetitively on labor were investigated in the subjects. In addition, to evaluate the level of degenerative change of the cervical spine on 83 people in the flexion group (flexion strain) and 83 people in the extension group (extension strain), cervical degenerative index (CDI) in the simple cervical spine lateral radiograph was used to score (0-60 points) the degenerative severity.
RESULTS
A total of 166 subjects (flexion group: 83 people, extension group: 83 people) participated in this study, and for the CDI, the cervical spine flexion group scored 7.8±6.2 points, and the cervical spine extension group scored 12.2±6.0 points to show that the cervical spine extension group had significant degenerative change in the cervical spine. In the multiple linear regression test performed to verify the risk factors affecting the degenerative change of the cervical spine, age (p=0.004), contraction of DM (p=0.029), and extension posture of cervical spine (p<0.001) influenced the degenerative change of the cervical spine.
CONCLUSION
Repetitive extension posture on the cervical spine on labor and contraction of diabetes affected degenerative change of the cervical spine, therefore, training in medical care and posture on labor are required to prevent the progression of degenerative change in the cervical spine.
Keyword
MeSH Terms
Figure
Reference
-
1. Ebersold MJ, Pare MC, Quast LM. Surgical treatment for cervical spondylitic myelopathy. J Neurosurg. 1995; 82:745–751.
Article2. Ferguson RJ, Caplan LR. Cervical spondylitic myelopathy. Neurol Clin. 1985; 3:373–382.
Article3. Garfin SR. Cervical degenerative disorders: etiology, presentation, and imaging studies. Instr Course Lect. 2000; 49:335–338.4. Buckwalter JA. Aging and degeneration of the human intervertebral disc. Spine (Phila Pa 1976). 1995; 20:1307–1314.
Article5. Lestini WF, Wiesel SW. The pathogenesis of cervical spondylosis. Clin Orthop Relat Res. 1989; 239:69–93.
Article6. Penning L. Some aspects of plain radiography of the cervical spine in chronic myelopathy. Neurology. 1962; 12:513–519.
Article7. Harrison DE, Harrison DD, Harrison SO, Troyanovich SJ. A review of biomechanics of the central nervous system. Part 1: spinal canal deformations caused by changes in posture. J Manipulative Physiol Ther. 2000; 23:217–220.8. Adams MA, Hutton WC. The effect of posture on the lumbar spine. J Bone Joint Surg Br. 1985; 67:625–629.
Article9. Penning L, Wilmink JT. Posture-dependent bilateral compression of L4 or L5 nerve roots in facet hypertrophy. A dynamic CT-myelographic study. Spine (Phila Pa 1976). 1987; 12:488–500.10. Ramos G, Martin W. Effects of vertebral axial decompression on intradiscal pressure. J Neurosurg. 1994; 81:350–353.
Article11. Dai LY, Xu YK, Zhang WM, Zhou ZH. The effect of flexionextension motion of the lumbar spine on the capacity of the spinal canal. An experimental study. Spine (Phila Pa 1976). 1989; 14:523–523.12. Adams MA, Dolan P, Hutton WC. The lumbar spine in backward bending. Spine (Phila Pa 1976). 1988; 13:1019–1026.
Article13. Takamiya Y, Nagata K, Fukuda K, Shibata A, Ishitake T, Suenaga T. Cervical spine disorders in farm workers requiring neck extension actions. J Orthop Sci. 2006; 11:235–240.
Article14. Ofiram E, Garvey TA, Schwender JD, et al. Cervical degenerative index: a new quantitative radiographic scoring system for cervical spondylosis with interobserver and intraobserver reliability testing. J Orthop Traumatol. 2009; 10:21–26.
Article15. Fujiwara A, Lim TH, An HS, et al. The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine (Phila Pa 1976). 2000; 25:3036–3044.
Article16. Hayashi H, Okada K, Hamada M, Tada K, Ueno R. Etiologic factors of myelopathy. A radiographic evaluation of the aging changes in the cervical spine. Clin Orthop Relat Res. 1987; 214:200–209.17. Emery SE. Cervical spondylotic myelopathy: diagnosis and treatment. J Am Acad Orthop Surg. 2001; 9:376–388.
Article18. Saunders RL, Wilson DH. The surgery of cervical disk disease: new perspectives. Clin Orthop Relat Res. 1980; 146:119–127.19. Anderson WW, Wise BL, Itabashi HH, Jones M. Cervical spondylosis in patients with athetosis. Neurology. 1962; 12:410–412.
Article20. Ebara S, Harada T, Yamazaki Y, et al. Unstable cervical spine in athetoid cerebral palsy. Spine (Phila Pa 1976). 1989; 14:1154–1159.
Article21. Wada E, Ebara S, Saito S, Ono K. Experimental spondylosis in the rabbit spine. Overuse could accelerate the spondylosis. Spine(Phila Pa 1976). 1992; 17:S1–S6.22. Jäger HJ, Gordon-Harris L, Mehring UM, Goetz GF, Mathias KD. Degenerative change in the cervical spine and loadcarrying on the head. Skeletal Radiol. 1997; 26:475–481.
Article23. Gill K, Videman T, Shimizu T, Mooney V. The effect of repeated extensions on the discographic dye patterns in cadaveric lumbar motion segments. Clin Biomech (Bristol, Avon). 1987; 2:205–210.
Article24. Edwards WC, LaRocca H. The developmental segmental sagittal diameter of the cervical spinal canal in patients with cervical spondylosis. Spine (Phila Pa 1976). 1983; 8:20–27.
Article25. Singh S, Kumar D, Kumar S. Risk factors in cervical spondylosis. J Clin Orthop Trauma. 2014; 5:221–226.
Article26. Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010; 87:4–14.
Article27. Machino M, Yukawa Y, Ito K, et al. Impact of diabetes on the outcomes of cervical laminoplasty: a prospective cohort study of more than 500 patients with cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2014; 39:220–227.28. Machino M, Yukawa Y, Ito K, et al. Risk factors for poor outcome of cervical laminoplasty for cervical spondylotic myelopathy in patients with diabetes. J Bone Joint Surg Am. 2014; 96:2049–2055.
Article29. Hájková Z, Streda A, Skrha F. Hyperostotic spondylosis and diabetes mellitus. Ann Rheum Dis. 1965; 24:536–543.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Kinematic Analysis of the Cervical Cord and Cervical Canal by Dynamic Neck Motion
- The Influence of Changes in Cervical Lordosis on Bulging Disk and Spinal Stenosis: Functional MR Imaging
- A Case of Quadriplegia after Parotidectomy in a Patient with Asymptomatic Cervical Spondylosis
- A Comparison Study of Cervical Flexion-Relaxation Ratio in the Normal and Forward Head Postures
- The Influence of Cervical Spondylosis to Acute Cervical Spinal Cord Injury