Korean J Gastroenterol.
2016 Jun;67(6):332-336. 10.4166/kjg.2016.67.6.332.
A Case of Adenomyomatous Hyperplasia of the Distal Common Bile Duct Mimicking Malignant Stricture
- Affiliations
-
- 1Department of Internal Medicine and Liver Research Institute, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. gidoctor@snuh.org
- KMID: 2307761
- DOI: http://doi.org/10.4166/kjg.2016.67.6.332
Abstract
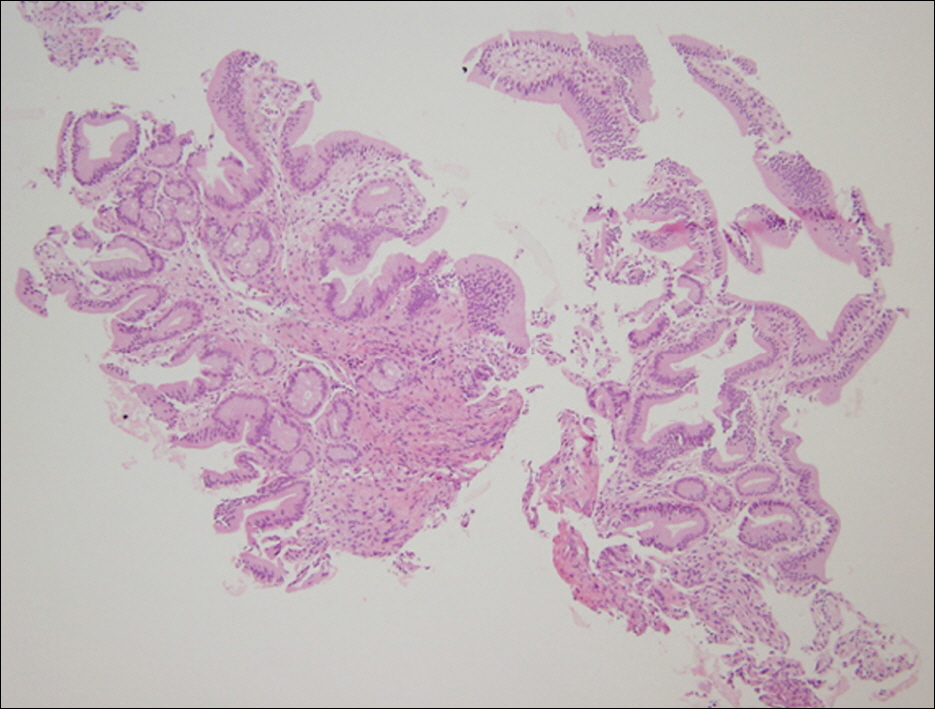
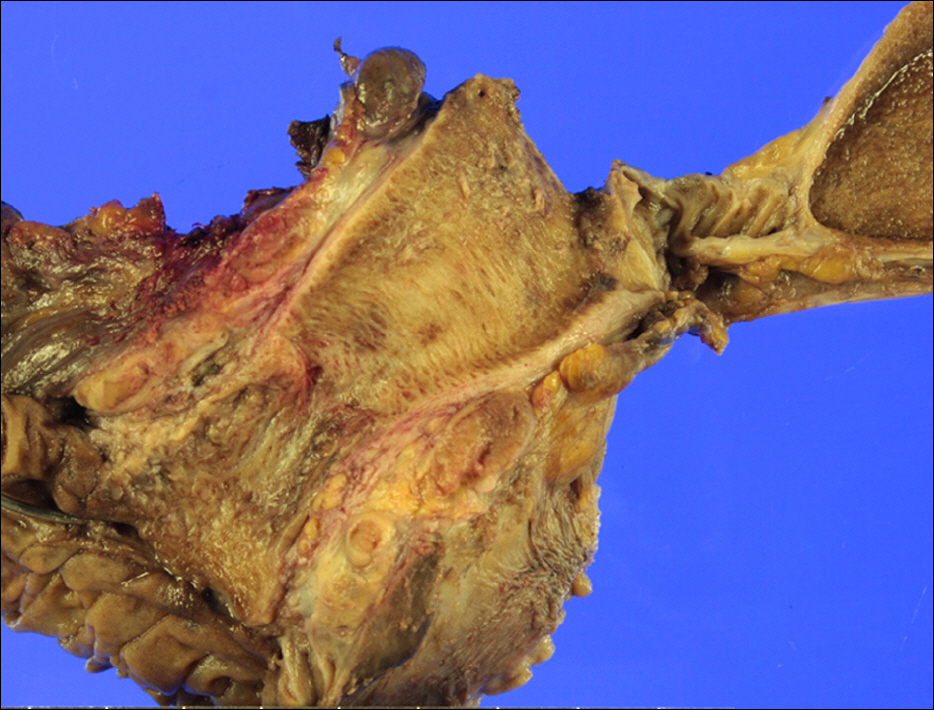
- Adenomyomatous hyperplasia is a reactive malformation or non-neoplastic tumor-like lesion frequently observed in the gallbladder, stomach, duodenum and jejunum, but rare in the extrahepatic bile duct. A 42-year-old man with epigastric discomfort had a stricture in the common bile duct on initial CT scans. Initially, it was regarded as a malignant lesion with some evidence, but histopathologic examinations of multiple biopsies obtained by multiple sessions of endoscopic retrograde cholangiopancreatography showed no evidence of malignancy. The patient had undergone the pylorus preserving pancreaticoduodenectomy because of the possibility of malignancy; however, the final diagnosis was adenomyomatous hyperplasia. It is important to distinguish a malignancy from benign biliary stricture with endoscopic biopsies. Surgery for suspected biliary malignancy often reveals benign lesions. Therefore, a correct diagnosis is important before deciding upon treatment of bile duct stricture. In conclusion, in younger patients with bile duct stricture where there is no evidence of histologic malignancy despite multiple biopsies, the possibility of benign disease such as adenomyomatous hyperplasia should be considered, to avoid unnecessary radical surgery.
MeSH Terms
Figure
Reference
-
References
1. Ozgonul A, Bitiren M, Guldur ME, Sogut O, Yilmaz LE. Fundal variant adenomyomatosis of the gallbladder: report of three cases and review of the literature. J Clin Med Res. 2010; 2:150–153.
Article2. Iwaki K, Shibata K, Ohta M, et al. Adenomyomatous hyperplasia of the common bile duct: report of a case. Surg Today. 2008; 38:85–89.
Article3. Jang KT, Heo JS, Choi SH, et al. Adenomyoma of ampulla of vater or the common bile duct: a report of three cases. Korean J Pathol. 2005; 39:59–62.4. Boggi U, Amorese G, Vistoli F, et al. Laparoscopic pancreaticoduodenectomy: a systematic literature review. Surg Endosc. 2015; 29:9–23.
Article5. Leichtle SW, Kaoutzanis C, Mouawad NJ, et al. Classic whipple versus pylorus-preserving pancreaticoduodenectomy in the ACS NSQIP. J Surg Res. 2013; 183:170–176.
Article6. Imai S, Uchiyama S, Suzuki T, et al. Adenomyoma of the common hepatic duct. J Gastroenterol. 1995; 30:547–550.
Article7. Kim JH, Jeong IH, Han JH, et al. Clinical/pathological analysis of gallbladder adenomyomatosis; type and pathogenesis. Hepatogastroenterology. 2010; 57:420–425.8. Patel S, Slade J, Jakate S. An unusual case of noninvasive adenocarcinoma arising in a localized adenomyoma of the gallbladder and review of literature. Int J Surg Pathol. 2016; 24:341–346.
Article9. Nishimura A, Shirai Y, Hatakeyama K. Segmental adenomyomatosis of the gallbladder predisposes to cholecystolithiasis. J Hepatobiliary Pancreat Surg. 2004; 11:342–347.
Article10. Singh A, Gelrud A, Agarwal B. Biliary strictures: diagnostic considerations and approach. Gastroenterol Rep (Oxf). 2015; 3:22–31.
Article11. Henson DE, Schwartz AM, Nsouli H, Albores-Saavedra J. Carcinomas of the pancreas, gallbladder, extrahepatic bile ducts, and ampulla of vater share a field for carcinogenesis: a population-based study. Arch Pathol Lab Med. 2009; 133:67–71.
Article12. Navaneethan U, Njei B, Lourdusamy V, Konjeti R, Vargo JJ, Parsi MA. Comparative effectiveness of biliary brush cytology and intraductal biopsy for detection of malignant biliary strictures: a systematic review and metaanalysis. Gastrointest Endosc. 2015; 81:168–176.
Article13. Kim JY, Choi JH, Kim JH, et al. Clinical usefulness of bile cytology obtained from biliary drainage tube for diagnosing cholangiocarcinoma. Korean J Gastroenterol. 2014; 63:107–113.
Article14. Uchida N, Kamada H, Ono M, et al. How many cytological examinations should be performed for the diagnosis of malignant biliary stricture via an endoscopic nasobiliary drainage tube? J Gastroenterol Hepatol. 2008; 23:1501–1504.
Article15. Logrono R, Kurtycz DF, Molina CP, Trivedi VA, Wong JY, Block KP. Analysis of false-negative diagnoses on endoscopic brush cytology of biliary and pancreatic duct strictures: the experience at 2 university hospitals. Arch Pathol Lab Med. 2000; 124:387–392.16. Voigtländer T, Lankisch TO. Endoscopic diagnosis of cholangiocarcinoma: From endoscopic retrograde cholangiography to bile proteomics. Best Pract Res Clin Gastroenterol. 2015; 29:267–275.
Article17. Navaneethan U, Hasan MK, Lourdusamy V, Njei B, Varadarajulu S, Hawes RH. Single-operator cholangioscopy and targeted biopsies in the diagnosis of indeterminate biliary strictures: a systematic review. Gastrointest Endosc. 2015; 82:608–614.e602.
Article18. Levy MJ, Baron TH, Clayton AC, et al. Prospective evaluation of advanced molecular markers and imaging techniques in patients with indeterminate bile duct strictures. Am J Gastroenterol. 2008; 103:1263–1273.
Article19. Domagk D, Poremba C, Dietl KH, et al. Endoscopic transpapillary biopsies and intraductal ultrasonography in the diagnostics of bile duct strictures: a prospective study. Gut. 2002; 51:240–244.
Article20. Navaneethan U, Njei B, Venkatesh PG, Lourdusamy V, Sanaka MR. Endoscopic ultrasound in the diagnosis of cholangiocarcinoma as the etiology of biliary strictures: a systematic review and metaanalysis. Gastroenterol Rep (Oxf). 2015; 3:209–215.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Leiomyoma in the Common Bile Duct
- A Case of Cutaneous Metastasis of Distal Common Bile Duct Carcinoma
- A Case of Multiple Papillary Adenocarcinoma of the Extrahepatic Bile Duct : Findings of ERCP
- A case of fascioliasis in common bile duct
- A Case of Villous Adenomas in the Common Bile Duct and Cystic Duct