J Korean Med Assoc.
2016 Jun;59(6):459-466. 10.5124/jkma.2016.59.6.459.
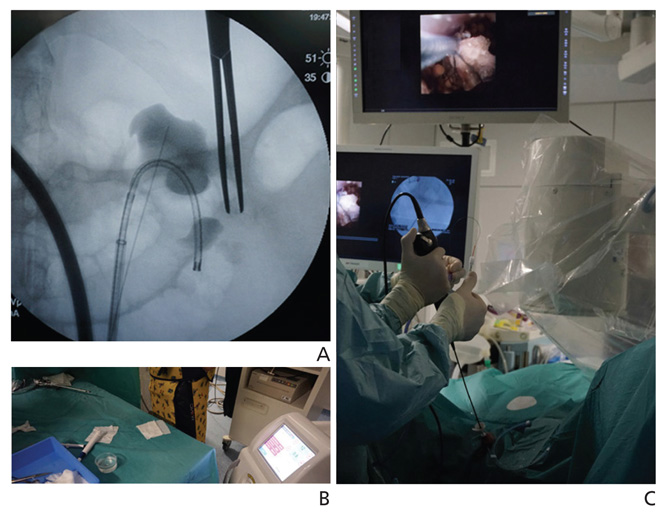
Current status of minimally invasive surgery for treatment of renal stones and tumors using a flexible ureteroscopy
- Affiliations
-
- 1Department of Urology, SMG-SNU Boramae Medical Center, Seoul, Korea. volley@snu.ac.kr
- KMID: 2305547
- DOI: http://doi.org/10.5124/jkma.2016.59.6.459
Abstract
- Retrograde intrarenal surgery (RIRS) has been accepted as the first-line option for surgical treatment of upper urinary tract pathologies including stones and tumors. With the development of surgical instruments with improved deflection mechanisms, visualization, and durability, RIRS has taken on an expanding role in treating urinary calculi located in the upper urinary tract, as it compensates for the shortcomings of shockwave lithotripsy and percutaneous nephrolithotomy. RIRS can also be considered a conservative treatment option for upper urinary tract urothelial cancer or as a means of intensive postoperative surveillance after radical treatment of urinary tract urothelial cancer. RIRS has a steep learning curve and various surgical techniques can be utilized during operations. The use of particular surgical instruments should take into consideration of the gain in surgical efficiency, decrease in complications, and cost-benefit tradeoff.
MeSH Terms
Figure
Reference
-
1. Marshall VF. Fiber optics in urology. J Urol. 1964; 91:110–114.
Article2. Bagley D, Erhard M. Use of the holmium laser in the upper urinary tract. Tech Urol. 19951; 25–30.3. Conlin MJ, Marberger M, Bagley DH. Ureteroscopy: development and instrumentation. Urol Clin North Am. 1997; 24:25–42.4. Shah K, Monga M, Knudsen B. Prospective randomized trial comparing 2 flexible digital ureteroscopes: ACMI/Olympus Invisio DUR-D and Olympus URF-V. Urology. 2015; 85:1267–1271.
Article5. Traxer O, Geavlete B, de Medina SG, Sibony M, Al-Qahtani SM. Narrow-band imaging digital flexible ureteroscopy in detection of upper urinary tract transitional-cell carcinoma: initial experience. J Endourol. 2011; 25:19–23.
Article6. Turk C, Knoll T, Petrik A, Sarica K, Skolarikos A, Straub M, Seitz C. Guidelines on urolithiasis [Internet]. Arnhem: European Association of Urology;2014. cited 2015 Jan 5. Available from: http://uroweb.org/guideline/urolithiasis/.7. Argyropoulos AN, Tolley DA. Evaluation of outcome following lithotripsy. Curr Opin Urol. 2010; 20:154–158.
Article8. Danuser H, Muller R, Descoeudres B, Dobry E, Studer UE. Extracorporeal shock wave lithotripsy of lower calyx calculi: how much is treatment outcome influenced by the anatomy of the collecting system? Eur Urol. 2007; 52:539–546.
Article9. Aboumarzouk OM, Monga M, Kata SG, Traxer O, Somani BK. Flexible ureteroscopy and laser lithotripsy for stones >2 cm: a systematic review and meta-analysis. J Endourol. 2012; 26:1257–1263.
Article10. Handa RK, Bailey MR, Paun M, Gao S, Connors BA, Willis LR, Evan AP. Pretreatment with low-energy shock waves induces renal vasoconstriction during standard shock wave lithotripsy (SWL): a treatment protocol known to reduce SWL-induced renal injury. BJU Int. 2009; 103:1270–1274.
Article11. Olvera-Posada D, Tailly T, Alenezi H, Violette PD, Nott L, Denstedt JD, Razvi H. Risk factors for postoperative complications of percutaneous nephrolithotomy at a tertiary referral center. J Urol. 2015; 194:1646–1651.
Article12. Kyriazis I, Panagopoulos V, Kallidonis P, Ozsoy M, Vasilas M, Liatsikos E. Complications in percutaneous nephrolithotomy. World J Urol. 2015; 33:1069–1077.
Article13. Chubak B, Stern JM. An unusual presentation of colon perforation following percutaneous nephrolithotomy. Can Urol Assoc J. 2014; 8:E862–E866.
Article14. Keeley FX Jr, Tilling K, Elves A, Menezes P, Wills M, Rao N, Feneley R. Preliminary results of a randomized controlled trial of prophylactic shock wave lithotripsy for small asymptomatic renal calyceal stones. BJU Int. 2001; 87:1–8.
Article15. Cho SY, Choo MS, Jung JH, Jeong CW, Oh S, Lee SB, Son H, Jeong H. Cumulative sum analysis for experiences of a single-session retrograde intrarenal stone surgery and analysis of predictors for stone-free status. PLoS One. 2014; 9:e84878.
Article16. Wilhelm K, Hein S, Adams F, Schlager D, Miernik A, Schoenthaler M. Ultra-mini PCNL versus flexible ureteroscopy: a matched analysis of analgesic consumption and treatment-related patient satisfaction in patients with renal stones 10-35 mm. World J Urol. 2015; 33:2131–2136.
Article17. Alkan E, Avci E, Ozkanli AO, Acar O, Balbay MD. Same-session bilateral retrograde intrarenal surgery for upper urinary system stones: safety and efficacy. J Endourol. 2014; 28:757–762.
Article18. Goldberg H, Holland R, Tal R, Lask DM, Livne PM, Lifshitz DA. The impact of retrograde intrarenal surgery for asymptomatic renal stones in patients undergoing ureteroscopy for a symptomatic ureteral stone. J Endourol. 2013; 27:970–973.
Article19. Zhang W, Zhou T, Wu T, Gao X, Peng Y, Xu C, Chen Q, Song R, Sun Y. Retrograde intrarenal surgery versus percutaneous nephrolithotomy versus extracorporeal shockwave lithotripsy for treatment of lower pole renal stones: a meta-analysis and systematic review. J Endourol. 2015; 29:745–759.
Article20. Ozturk U, Sener NC, Goktug HN, Nalbant I, Gucuk A, Imamoglu MA. Comparison of percutaneous nephrolithotomy, shock wave lithotripsy, and retrograde intrarenal surgery for lower pole renal calculi 10-20 mm. Urol Int. 2013; 91:345–349.
Article21. Aboumarzouk OM, Somani BK, Monga M. Flexible ureteroscopy and holmium:YAG laser lithotripsy for stone disease in patients with bleeding diathesis: a systematic review of the literature. Int Braz J Urol. 2012; 38:298–305.
Article22. Leavitt DA, Theckumparampil N, Moreira DM, Elsamra SE, Waingankar N, Hoenig DM, Smith AD, Okeke Z. Continuing aspirin therapy during percutaneous nephrolithotomy: unsafe or under-utilized? J Endourol. 2014; 28:1399–1403.
Article23. Zhong W, Yang B, He F, Wang L, Swami S, Zeng G. Surgical management of urolithiasis in patients after urinary diversion. PLoS One. 2014; 9:e111371.
Article24. Stuurman RE, Al-Qahtani SM, Cornu JN, Traxer O. Antegrade percutaneous flexible endoscopic approach for the management of urinary diversion-associated complications. J Endourol. 2013; 27:1330–1334.
Article25. Orihuela E, Smith AD. Percutaneous treatment of transitional cell carcinoma of the upper urinary tract. Urol Clin North Am. 1988; 15:425–431.
Article26. Bagley DH, Grasso M 3rd. Ureteroscopic laser treatment of upper urinary tract neoplasms. World J Urol. 2010; 28:143–149.
Article27. Stewart GD, Bariol SV, Grigor KM, Tolley DA, McNeill SA. A comparison of the pathology of transitional cell carcinoma of the bladder and upper urinary tract. BJU Int. 2005; 95:791–793.
Article28. Yamany T, van Batavia J, Ahn J, Shapiro E, Gupta M. Ureterorenoscopy for upper tract urothelial carcinoma: how often are we missing lesions? Urology. 2015; 85:311–315.
Article29. Jung JW, Lee BK, Park YH, Lee S, Jeong SJ, Lee SE, Jeong CW. Modified Seoul National University Renal Stone Complexity score for retrograde intrarenal surgery. Urolithiasis. 2014; 42:335–340.
Article30. Park J, Kang M, Jeong CW, Oh S, Lee JW, Lee SB, Son H, Jeong H, Cho SY. External validation and evaluation of reliability and validity of the modified Seoul National University Renal Stone Complexity Scoring System to predict stone-free status after retrograde intrarenal surgery. J Endourol. 2015; 29:888–893.
Article31. De S, Autorino R, Kim FJ, Zargar H, Laydner H, Balsamo R, Torricelli FC, Di Palma C, Molina WR, Monga M, De Sio M. Percutaneous nephrolithotomy versus retrograde intrarenal surgery: a systematic review and meta-analysis. Eur Urol. 2015; 67:125–137.
Article32. Chou YH, Li CC, Hsu H, Chang WC, Liu CC, Li WM, Ke HL, Lee MH, Liu ME, Pan SC, Wang HS. Renal function in patients with urinary stones of varying compositions. Kaohsiung J Med Sci. 2011; 27:264–267.
Article33. Giusti G, Proietti S, Cindolo L, Peschechera R, Sortino G, Berardinelli F, Taverna G. Is retrograde intrarenal surgery a viable treatment option for renal stones in patients with solitary kidney? World J Urol. 2015; 33:309–314.
Article34. Piao S, Park J, Son H, Jeong H, Cho SY. Evaluation of renal function in patients with a main renal stone larger than 1 cm and perioperative renal functional change in minimally invasive renal stone surgery: a prospective, observational study. World J Urol. 2016; 34:725–732.
Article35. Netsch C, Knipper S, Bach T, Herrmann TR, Gross AJ. Impact of preoperative ureteral stenting on stone-free rates of ureteroscopy for nephroureterolithiasis: a matched-paired analysis of 286 patients. Urology. 2012; 80:1214–1219.
Article36. Chu L, Farris CA, Corcoran AT, Averch TD. Preoperative stent placement decreases cost of ureteroscopy. Urology. 2011; 78:309–313.
Article37. Lange D, Bidnur S, Hoag N, Chew BH. Ureteral stent-associated complications: where we are and where we are going. Nat Rev Urol. 2015; 12:17–25.
Article38. Traxer O, Wendt-Nordahl G, Sodha H, Rassweiler J, Meretyk S, Tefekli A, Coz F, de la Rosette JJ. Differences in renal stone treatment and outcomes for patients treated either with or without the support of a ureteral access sheath: the Clinical Research Office of the Endourological Society Ureteroscopy Global Study. World J Urol. 2015; 33:2137–2144.
Article39. Berquet G, Prunel P, Verhoest G, Mathieu R, Bensalah K. The use of a ureteral access sheath does not improve stone-free rate after ureteroscopy for upper urinary tract stones. World J Urol. 2014; 32:229–232.
Article40. Ng YH, Somani BK, Dennison A, Kata SG, Nabi G, Brown S. Irrigant flow and intrarenal pressure during flexible ureteroscopy: the effect of different access sheaths, working channel instruments, and hydrostatic pressure. J Endourol. 2010; 24:1915–1920.
Article41. Sarkissian C, Noble M, Li J, Monga M. Patient decision making for asymptomatic renal calculi: balancing benefit and risk. Urology. 2013; 81:236–240.
Article42. Mogilevkin Y, Sofer M, Margel D, Greenstein A, Lifshitz D. Predicting an effective ureteral access sheath insertion: a bicenter prospective study. J Endourol. 2014; 28:1414–1417.
Article43. Chan KF, Vassar GJ, Pfefer TJ, Teichman JM, Glickman RD, Weintraub ST, Welch AJ. Holmium:YAG laser lithotripsy: a dominant photothermal ablative mechanism with chemical decomposition of urinary calculi. Lasers Surg Med. 1999; 25:22–37.
Article44. Prabhakar M. Retrograde ureteroscopic intrarenal surgery for large (1.6-3.5 cm) upper ureteric/renal calculus. Indian J Urol. 2010; 26:46–49.
Article45. Hamamoto S, Yasui T, Okada A, Koiwa S, Taguchi K, Itoh Y, Kawai N, Hashimoto Y, Tozawa K, Kohri K. Efficacy of endoscopic combined intrarenal surgery in the prone split-leg position for staghorn calculi. J Endourol. 2015; 29:19–24.
Article46. Traxer O, Letendre J. Extracorporeal lithotripsy endoscopically controlled by ureterorenoscopy (LECURS): a new concept for the treatment of kidney stones-first clinical experience using digital ureterorenoscopes. World J Urol. 2014; 32:715–721.
Article47. Palmero JL, Miralles J, Garau C, Nuno de la Rosa I, Amoros A, Benedicto A. Retrograde intrarenal surgery (RIRS) in the treatment of calyceal diverticulum with lithiasis. Arch Esp Urol. 2014; 67:331–336.48. Saglam R, Muslumanoglu AY, Tokatlı Z, Caşkurlu T, Sarica K, Taşçi AI, Erkurt B, Suer E, Kabakci AS, Preminger G, Traxer O, Rassweiler JJ. A new robot for flexible ureteroscopy: development and early clinical results (IDEAL stage 1-2b). Eur Urol. 2014; 66:1092–1100.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antegrade Flexible Ureteroscopy for Bilateral Ureteral Stones in a Patient with Severe Hip Joint Ankylosis
- Flexible Ureterorenoscopy in the Upper Urinary Tract Diseases
- The usefulness and ergonomics of a new robotic system for flexible ureteroscopy and laser lithotripsy for treating renal stones
- Efficacy of Percutaneous Nephrostomy During Flexible Ureteroscopy for Renal Stone Management
- Effectiveness of Flexible Ureteroscopic Stone Removal for Treating Ureteral and Ipsilateral Renal Stones: A Single-Center Experience