Korean J Urol.
2006 Aug;47(8):876-881. 10.4111/kju.2006.47.8.876.
Precise Anatomical Location of the Autonomous Nerve from the Pelvic Plexus to the Corpus Cavernosum
- Affiliations
-
- 1Department of Urology, Gangneung Asan Hospital, College of Medicine, Ulsan University, Korea. jypark@gnah.co.kr
- 2Department of Anatomy, College of Medicine, Kwandong University, Gangneung, Korea.
- KMID: 2294118
- DOI: http://doi.org/10.4111/kju.2006.47.8.876
Abstract
-
PURPOSE: We wanted to study the precise anatomical location of the branches of the pelvic plexus from the sacral root to the cavernous nerve.
MATERIALS AND METHODS
We performed microdissection on the pelvises from 4 male formalin fixed cadavers under a Zeiss surgical microscope and we traced the location of the branches of the pelvic plexus at a magnification of 6x.
RESULTS
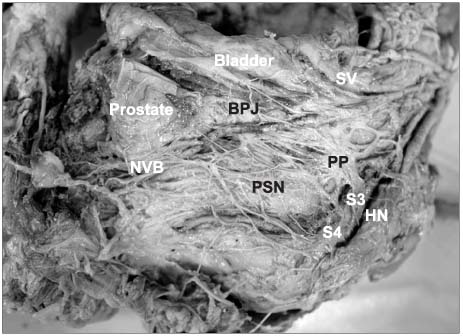
The configuration of the pelvic plexus was an irregular diamond shape rather than rectangular. It was located retroperitoneally on the lateral wall of the rectum 8.2 to 11.5cm from the anal verge. Its midpoint was located 2.0 to 2.5cm from the seminal vesicle posterosuperiorly. A prominent neurovascular bundle (NVB) was located on the posterolateral portion of the apex and the mid portion of the prostate. The pelvic splanchnic nerve (PSN) joined the NVB at a point distal and inferior to the bladder-prostate (BP) junction. The PSN components joined the NVB in a spray-like distribution at multiple levels distal to the BP junction. The distance from the membranous urethra to the NVB was 0.5 to 1.2cm. We also found multiple tiny branches on the anterolateral aspect of the prostate apex.
CONCLUSIONS
In contrast to the usual concept, the NVB was much wider above the mid portion of the prostrate and it supplied multiple tiny branches on the anterolateral aspect of the prostate. The PSN branches arose from the more posteroinferior area of the pelvic plexus. Therefore, we recommend a more anterior dissection of the lateral pelvic fascia for nerve sparing radical prostatectomy. If surgeons plan a nerve graft after radical prostatectomy, they should consider this neuroanatomy for obtaining a successful outcome.
Keyword
MeSH Terms
Figure
Reference
-
1. Walsh PC, Lepor H, Eggleston JC. Radical prostatectomy with preservation of sexual function: anatomical and pathological considerations. Prostate. 1983. 4:473–485.2. Schlegel PN, Walsh PC. Neuroanatomical approach to radical cystoprostatectomy with preservation of sexual function. J Urol. 1987. 138:1402–1406.3. Catalona WJ, Dresner SM. Nerve-sparing radical prostatectomy: extraprostatic tumour extension and preservation of erectile function. J Urol. 1986. 134:1149.4. Turk IA, Deger S, Morgan WR, Davis JW, Schellhammer PF, Loening SA. Sural nerve graft during laparoscopic radical prostatectomy. Initial experience. Urol Oncol. 2002. 7:191–194.5. Kourambas J, Angus DG, Hosking P, Chou ST. A histological study of Denonvilliers' fascia and its relationship to the neurovascular bundle. Br J Urol. 1998. 82:408–410.6. Lunacek A, Schwentner C, Fritsch H, Bartsch G, Strasser H. Anatomical radical retropubic prostatectomy: 'curtain dissection' of the neurovascular bundle. BJU Int. 2005. 95:1226–1231.7. Baader B, Herrmann M. Topography of the pelvic autonomic nervous system and its potential impact on surgical intervention in the pelvis. Clin Anat. 2003. 16:119–130.8. Takenaka A, Murakami G, Soga H, Han SH, Arai Y, Fujisawa M. Anatomical analysis of the neurovascular bundle supplying penile cavernous tissue to ensure a reliable nerve graft after radical prostatectomy. J Urol. 2004. 172:1032–1035.9. Walsh PC, Donker PJ. Impotence following radical prostatectomy: insight into etiology and prevention. J Urol. 1982. 128:492–497.10. Lepor H, Gregerman M, Crosby R, Mostofi FK, Walsh PC. Precise localization of the autonomic nerves from the pelvic plexus to the corpora cavernosa: a detailed anatomical study of the adult male pelvis. J Urol. 1985. 133:207–212.11. Kim ED, Nath R, Kadmon D, Lipshultz LI, Miles BJ, Slawin KM, et al. Bilateral nerve graft during radical retropubic prostatectomy: 1-year follow up. J Urol. 2001. 165:1950–1956.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pharmacologic Effect of Phentolamine on Norepinephrine Induced Contraction of Corpus Cavernosum
- A New Technique for Inferior Hypogastric Plexus Block: A Coccygeal Transverse Approach: A Case Report
- A Case or Priapism Treated by Corpus Cavernosum-Saphenous Vein Anastomosis
- A Case of Penile Injury (Accidental Rupture of Corpus Cavernosum)
- A Fibrotic Nodule in the Corpus Cavernosum