J Korean Ophthalmol Soc.
2016 Jun;57(6):957-962. 10.3341/jkos.2016.57.6.957.
Diagnostic Availability of Blind Spot Mapping for Ocular Torsion
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea. yclee@cmcnu.or.kr
- 2Department of Ophthalmology, Konyang University College of Medicine, Daejeon, Korea.
- 3Department of Ophthalmology, Keimyung University School of Medicine, Daegu, Korea.
- KMID: 2290499
- DOI: http://doi.org/10.3341/jkos.2016.57.6.957
Abstract
- PURPOSE
To evaluate diagnostic the usefulness of blind spot mapping in measuring ocular torsion changes and to investigate the correlations of inferior oblique muscle overaction (IOOA) and excyclotorsion measurements using fundus photographs and blind spot mapping in patients with secondary IOOA.
METHODS
Eleven patients (12 eyes; IOOA group) diagnosed with secondary IOOA were evaluated for ocular movement, fundus photograph and Humphrey standard automated perimetry, and 10 patients (20 eyes; control group) were subjected to the same tests. An ocular movement examination was performed to evaluate IOOA, and fundus photograph and Humphrey standard automated perimetry were used to measure the ocular torsion. Inferior oblique myectomy or recession was performed along with horizontal strabismus surgery, and preoperative and postoperative IOOA and ocular torsion measurements were compared between the groups.
RESULTS
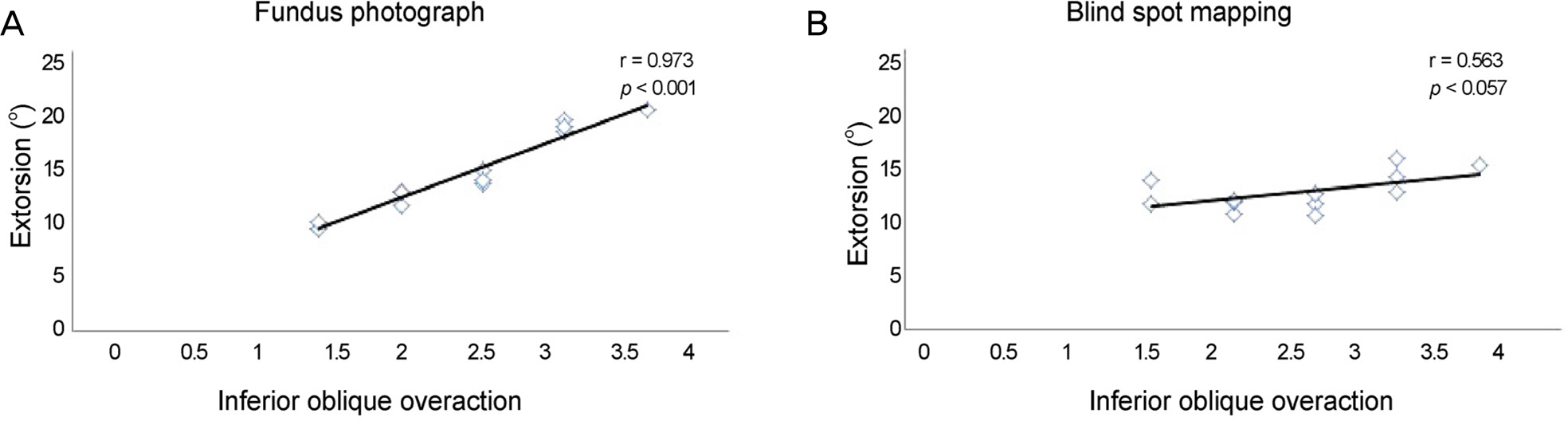
In the IOOA group after surgery, the IOOA decreased from +2.42 ± 0.63 to +0.50 ± 0.52, the ocular torsion decreased from +14.15 ± 3.60° to +7.47 ± 1.65° (p < 0.001) on fundus photographs, and from +12.19 ± 1.62° to +9.69 ± 1.75° (p = 0.061) in Humphrey standard automated perimetry. The control group showed a mean ocular torsion of 7.44 ± 1.62° on fundus photographs and +7.24 ± 1.28° on Humphrey standard automated perimetry.
CONCLUSIONS
The usefulness of blind spot mapping when the ocular torsion was measured in IOOA patients was considered low, due to the weak correlation between IOOA and extorsion; preoperative and postoperative ocular torsion amount values were not significantly different.
Figure
Reference
-
References
1. Knapp P. Vertically incomitant horizontal strabismus: the so-called “A” and “V” syndromes. Trans Am Ophthalmol Soc. 1959; 57:666–99.2. Bixenman WW, von Noorden GK. Apparent foveal displacement in normal subjects and in cyclotropia. Ophthalmology. 1982; 89:58–62.
Article3. Locke JC. Heterotopia of the blind spot in ocular vertical muscle imbalance. Am J Ophthalmol. 1968; 65:362–74.
Article4. Morton GV, Lucchese N, Kushner BJ. The role of funduscopy and fundus photography in strabismus diagnosis. Ophthalmology. 1983; 90:1186–91.
Article5. Lee HJ, Lim KH. The range of ocular torsion in mass screening. J Korean Ophthalmol Soc. 2005; 46:1684–9.6. Versino M, Newman-Toker DE. Blind spot heterotopia by abdominal static perimetry to assess static ocular torsion: centro-cecal axis rotation in normals. J Neurol. 2010; 257:291–3.7. Von Noorden GK, Campos EC. Binocular Vision and Ocular Motility: Theory and Management of Strabismus. 6th ed.St Louis: St Louis;2002. p. 55–6.8. Rosenbaum AL, Santiago AP. Clinical Strabismus Management. 1st ed.Philadelphia: Philadelphia;1999. p. 55–9.9. Kim EH, Lee SJ, Choi HY. Ocular torsion according to fixation in fundus photograph. J Korean Ophthalmol Soc. 2006; 47:449–54.10. Guyton DL. Clinical assessment of ocular torsion. Am Orthopt J. 1983; 33:85.
Article11. Eustis HS, Nussdorf JD. Inferior oblique overaction in infantile esotropia: fundus extorsion as a predictive sign. J Pediatr Ophthalmol Strabismus. 1996; 33:85–8.
Article12. Cho HH, Sohn MA. The ocular cyclotorsion induced by the abdominalal change. J Korean Ophthalmol Soc. 1999; 40:2911–7.13. Yim JH, Min BM, Xu YG. Surgical results of classic Harada-Ito procedure with intraoperative adjustment for excyclotorsion. J Korean Ophthalmol Soc. 2002; 43:2227–33.14. Sim JH, Lee SY. The effect of inferior oblique weakening abdominal on the correction of ocular torsion. J Korean Ophthalmol Soc. 2005; 46:1020–6.15. Lee DH, Lee SJ, Park SH. Ocular torsion in normal Korean population. J Korean Ophthalmol Soc. 2004; 45:797–802.16. Park SW. The torsional status of normal Koreans. J Korean Ophthalmol Soc. 2004; 45:1906–11.17. Ramat S, Nesti A, Versino M, et al. A new device to assess static ocular torsion. Ann N Y Acad Sci. 2011; 1233:226–30.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Age and Gender Specific Reference Value of Ocular Torsion by Using Funduscope in Korean
- Comparison of Diplopia and Ocular Torsion Rate in Blow-Out Fracture Patients
- Clinical Significance of Torsion Measured by Fundus Photography in Children
- Ocular Tilt Reaction
- The Clinical Significance of Torsion of Appendix Testis in Acute Scrotum