J Clin Neurol.
2008 Sep;4(3):111-115. 10.3988/jcn.2008.4.3.111.
Association of Initial Infarct Extent and Progressive Motor Deficits in Striatocapsular Infarction
- Affiliations
-
- 1Department of Neurology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. chungpw@hanmail.net
- 2Department of Neurosurgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Neurology, Chung-Ang University Medical Center, Chung-Ang University College of Medicine, Seoul, Korea.
- KMID: 2287674
- DOI: http://doi.org/10.3988/jcn.2008.4.3.111
Abstract
-
BACKGROUND AND PURPOSE: Progression of motor deficits in the acute period is frequently observed in patients with subcortical striatocapsular infarctions. Therefore, we sought to determine the factors associated with early motor progression in patients with infarcts confined to the striatocapsular region.
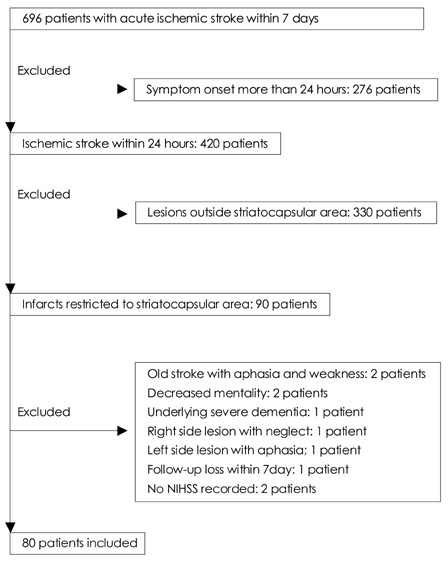
METHODS
We studied 80 consecutive patients with striatocapsular-region infarction, as defined by clinical and MRI criteria, within 24 hours after stroke onset. Motor progression was defined as an increase of >2 points in the motor items of the National Institutes of Health Stroke Scale (NIHSS) within 7 days of stroke onset. The study population was divided into patients with and without motor progression, and risk factors, clinical features, and brain MRI/magnetic resonance angiograpy (MRA) findings were compared between these groups.
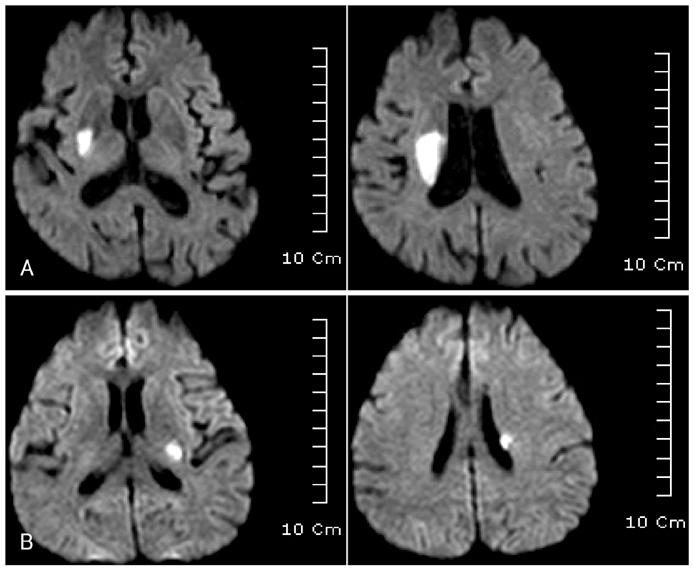
RESULTS
Motor progression was observed in 40% of the 80 patients. The independent variables associated with motor progression were a history of hypertension (OR=7.8, 95% CI=1.5-39.8, p=0.013) and an initial infarct extent of > or =15 mm (OR=9.2, 95% CI=1.8-45.7, p=0.006). However, there were no differences in the initial NIHSS score, other stroke risk factors, vascular stenosis pattern, or cardioembolic source.
CONCLUSIONS
Early motor progression in patients with striatocapsular-region infarction is associated with the initial extent of the lesion. However, the stroke mechanism and vascular stenosis did not differ between the motor progression and stable groups.
Keyword
MeSH Terms
Figure
Reference
-
1. Nakamura K, Saku Y, Ibayashi S, Fujishima M. Progressive motor deficits in lacunar infarction. Neurology. 1999. 52:29–33.
Article2. Serena J, Leira R, Castillo J, Pumar JM, Castellanos M, Dávalos A. Neurological deterioration in acute lacunar infarctions: the role of excitatory and inhibitory neurotransmitters. Stroke. 2001. 32:1154–1161.
Article3. Steinke W, Ley SC. Lacunar stroke is the major cause of progressive motor deficits. Stroke. 2002. 33:1510–1516.
Article4. Tatu L, Moulin T, Bogousslavsky J, Duvernoy H. Arterial territories of the human brain: cerebral hemispheres. Neurology. 1998. 50:1699–1708.
Article5. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993. 24:35–41.
Article6. Lyden P, Brott T, Tilley B, Welch KM, Mascha EJ, Levine S, et al. NINDS tPA Stroke Study Group. Improved reliability of the NIH Stroke Scale using video training. Stroke. 1994. 25:2220–2226.
Article7. Bladin PF, Berkovic SF. Striatocapsular infarction: large infarcts in the lenticulostriate arterial territory. Neurology. 1984. 34:1423–1430.
Article8. Adachi T, Kobayashi S, Yamaguchi S, Okada K. MRI findings of small subcortical "lacunar-like" infarction resulting from large vessel disease. J Neurol. 2000. 247:280–285.
Article9. Waterston JA, Brown MM, Butler P, Swash M. Small deep cerebral infarcts associated with occlusive internal carotid artery disease. A hemodynamic phenomenon? Arch Neurol. 1990. 47:953–957.
Article10. Cho AH, Kang DW, Kwon SU, Kim JS. Is 15 mm size criterion for lacunar infarction still valid? A study on strictly subcortical middle cerebral artery territory infarction using diffusion-weighted MRI. Cerebrovasc Dis. 2007. 23:14–19.
Article11. Han MK, Kang DW, Jeong SW, Roh JK. Aphasia following striatocapsular infarction may be explained by concomitant small cortical infarct on diffusion-weighted imaging. Cerebrovasc Dis. 2005. 19:220–224.
Article12. Bang OY, Yeo SH, Yoon JH, Seok JI, Sheen SS, Yoon SR, et al. Clinical MRI cutoff point for predicting lacunar stroke may not exist: need for a grading rather than a dichotomizing system. Cerebrovasc Dis. 2007. 24:520–529.
Article13. Marinkovic SV, Milisavljevic MM, Kovacevic MS, Stevic ZD. Perforating branches of the middle cerebral artery. Microanatomy and clinical significance of their intracerebral segments. Stroke. 1985. 16:1022–1029.
Article14. Umansky F, Gomes FB, Dujovny M, Diaz FG, Ausman JI, Mirchandani HG, et al. The perforating branches of the middle cerebral artery. A microanatomical study. J Neurosurg. 1985. 62:261–268.15. Aydin IH, Taçki E, Kadioğlu HH, Kayaoğlu CR, Tüzün Y. The variations of lenticulostriate arteries in the middle cerebral artery aneurysms. Acta Neurochir (Wien). 1996. 138:555–559.
Article16. Lodder J, Gorsselink EL. Progressive stroke caused by CT-verified small deep infarcts; relation with the size of the infarct and clinical outcome. Acta Neurol Scand. 1985. 71:328–330.
Article17. Bang OY, Heo JH, Kim JY, Park JH, Huh K. Middle cerebral artery stenosis is a major clinical determinant in striatocapsular small, deep infarction. Arch Neurol. 2002. 59:259–263.
Article18. Yamada K, Ito H, Nakamura H, Kizu O, Akada W, Kubota T, et al. Stroke patients' evolving symptoms assessed by tractography. J Magn Reson Imaging. 2004. 20:923–929.
Article19. Lansberg MG, O'Brien MW, Tong DC, Moseley ME, Albers GW. Evolution of cerebral infarct volume assessed by diffusion-weighted magnetic resonance imaging. Arch Neurol. 2001. 58:613–617.
Article20. Park KY, Youn YC, Chung CS, Lee KH, Kim GM, Chung PW, et al. Large-artery stenosis predicts subsequent vascular events in patients with transient ischemic attack. J Clin Neurol. 2007. 3:169–174.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Magnetic Resonance Angiographic Findings and Clinical Outcome of the Striatocapsular Infarction
- The Clinical Properties of Deep Small Basal Ganglia Infarctions: Lacune or Small Striatocapsular Infarction?
- Strategic Infarct Dementia after Bilateral Anterior Fornix Infarction
- Opalski Syndrome Presenting as Sensorimotor Deficits Ipsilateral to Cerebral Infarction
- Analysis of the Lesion Distributions and Mechanism of Acute Middle Cerebral Artery Infarctions Involving the Striatocapsular Region