J Clin Neurol.
2011 Sep;7(3):109-114. 10.3988/jcn.2011.7.3.109.
Disability-Adjusted Life Years Analysis: Implications for Stroke Research
- Affiliations
-
- 1Department of Neurology, Stroke Center, Ilsan Paik Hospital, Inje University, Goyang, Korea. nrhks@paik.ac.kr
- KMID: 2287625
- DOI: http://doi.org/10.3988/jcn.2011.7.3.109
Abstract
- Stroke is a prototype disorder that disables as well as kills people. The disability-adjusted life years (DALY) metric developed by the World Health Organization to measure the global burden of disease integrates healthy life years lost due to both premature mortality and living with disability. Accordingly, it is well suited to stroke research. The DALY has previously been applied only to large but relatively crude population-level data analyses, but now it is possible to calculate the DALY lost in individual stroke patients. Measuring each patient's stroke outcome with DALY lost has expanded its application to the analysis of treatment effect in acute stroke trials, delineating the poststroke complication impact, the differential weighting of discrete vascular events, and estimating a more refined stroke burden in a specific population. The DALY metric has several advantages over conventional stroke outcome measures: 1) Since the DALY measures the burden of diverse health conditions with a common metric of life years lost, stroke burden and benefits of stroke interventions can be directly compared to other health conditions and their treatments. 2) Quantifying stroke burden or interventional benefits as the life years lost or gained makes the DALY metric more intuitively accessible for public and health system planners. 3) As a continuous, equal-interval scale, the DALY analysis might be statistically more powerful than either binary or ordinal rank outcome analyses in detecting the treatment effects of clinical trials. 4) While currently employed stroke outcome measures take one-time snapshots of disability or mortality and implicitly indicate long-term health impact, the DALY explicitly indicates the burdens of living with disability for an individual's remaining life.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The economic burden of stroke in 2010 in Korea
Hyun-Jin Kim, Young-Ae Kim, Hye-Young Seo, Eun-Jung Kim, Seok-Jun Yoon, In-Hwan Oh
J Korean Med Assoc. 2012;55(12):1226-1236. doi: 10.5124/jkma.2012.55.12.1226.
Reference
-
1. Murray CJL. Murray CJL, Lopez AD, editors. Rethinking DALYs. The Global Burden of Disease. Vol 1 of Global Burden of Disease and Injury Series. 1996. Cambridge, MA: Harvard School of Public Health;1–98.2. The Global Burden of Disease: 2004 Update. WHO. Accessed 2009 Feb 4. Available from: http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/index.html.3. Global Burden of Disease 2004 Update: Disability Weights for Diseases and Conditions. WHO. Accessed 2009 Feb 4. Available from: www.who.int/healthinfo/global_burden_disease/GBD2004_DisabilityWeights.pdf.4. Ezzati M, Hoorn SV, Rodgers A, Lopez AD, Mathers CD, Murray CJ. Comparative Risk Assessment Collaborating Group. Estimates of global and regional potential health gains from reducing multiple major risk factors. Lancet. 2003. 362:271–280.
Article5. Moodie ML, Carter R, Mihalopoulos C, Thrift AG, Chambers BR, Donnan GA, et al. Trial application of a Model of Resource Utilization, Costs, and Outcomes for Stroke (MORUCOS) to assist priority setting in stroke. Stroke. 2004. 35:1041–1046.
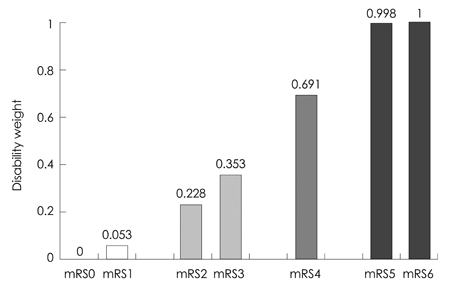
Article6. Hong KS, Saver JL. Quantifying the value of stroke disability outcomes: WHO global burden of disease project disability weights for each level of the modified Rankin Scale. Stroke. 2009. 40:3828–3833.
Article7. Hong KS, Saver JL. Years of disability-adjusted life gained as a result of thrombolytic therapy for acute ischemic stroke. Stroke. 2010. 41:471–477.
Article8. Hong KS, Saver JL, Kang DW, Bae HJ, Yu KH, Koo J, et al. Years of optimum health lost due to complications after acute ischemic stroke: disability-adjusted life-years analysis. Stroke. 2010. 41:1758–1765.
Article9. Eriksson M, Norrving B, Terént A, Stegmayr B. Functional outcome 3 months after stroke predicts long-term survival. Cerebrovasc Dis. 2008. 25:423–429.
Article10. Slot KB, Berge E, Dorman P, Lewis S, Dennis M, Sandercock P, et al. Impact of functional status at six months on long term survival in patients with ischaemic stroke: prospective cohort studies. BMJ. 2008. 336:376–379.
Article11. Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, et al. Second European-Australasian Acute Stroke Study Investigators. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Lancet. 1998. 352:1245–1251.
Article12. Ogawa A, Mori E, Minematsu K, Taki W, Takahashi A, Nemoto S, et al. Randomized trial of intraarterial infusion of urokinase within 6 hours of middle cerebral artery stroke: the middle cerebral artery embolism local fibrinolytic intervention trial (MELT) Japan. Stroke. 2007. 38:2633–2639.
Article13. Bae HJ, Yoon DS, Lee J, Kim BK, Koo JS, Kwon O, et al. In-hospital medical complications and long-term mortality after ischemic stroke. Stroke. 2005. 36:2441–2445.
Article14. Hong KS, Kang DW, Koo JS, Yu KH, Han MK, Cho YJ, et al. Impact of neurological and medical complications on 3-month outcomes in acute ischaemic stroke. Eur J Neurol. 2008. 15:1324–1331.
Article15. Sulter G, Elting JW, Langedijk M, Maurits NM, De Keyser J. Admitting acute ischemic stroke patients to a stroke care monitoring unit versus a conventional stroke unit: a randomized pilot study. Stroke. 2003. 34:101–104.
Article16. Hinchey JA, Shephard T, Furie K, Smith D, Wang D, Tonn S, et al. Formal dysphagia screening protocols prevent pneumonia. Stroke. 2005. 36:1972–1976.
Article17. Korea Centers for Disease Control and Prevention. Construction of National Surveillance System for Cardiovascular & Cerebrovascular Diseases. 2006.18. Brott TG, Hobson RW 2nd, Howard G, Roubin GS, Clark WM, Brooks W, et al. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med. 2010. 363:11–23.
Article19. Peeters A, Mamun AA, Willekens F, Bonneux L. A cardiovascular life history. A life course analysis of the original Framingham Heart Study cohort. Eur Heart J. 2002. 23:458–466.20. Hong KS, Ali LK, Selco SL, Fonarow GC, Saver JL. Weighting components of composite end points in clinical trials: an approach using disability-adjusted life-years. Stroke. 2011. 42:1722–1729.
Article21. Maddox TM, Reid KJ, Spertus JA, Mittleman M, Krumholz HM, Parashar S, et al. Angina at 1 year after myocardial infarction: prevalence and associated findings. Arch Intern Med. 2008. 168:1310–1316.
Article22. Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, et al. Heart disease and stroke statistics--2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009. 119:480–486.23. Johnston SC, Mendis S, Mathers CD. Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modelling. Lancet Neurol. 2009. 8:345–354.
Article24. Hong KS, Kim J, Cho YJ, Seo SY, Hwang SI, Kim SC, et al. Burden of ischemic stroke in Korea: analysis of disability-adjusted life years lost. J Clin Neurol. 2011. 7:77–84.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Study of Disability-Adjusted Life Expectancy(DALE) Using National Health Interview Survey in Korea
- The Burden of Stroke in Kurdistan Province, Iran From 2011 to 2017
- Relation of Stroke Risk Factors to Severity and Disability after Ischemic Stroke
- Impact of Poststroke Fatigue on Health-Related Quality of Life of Nigerian Stroke Survivors
- Review of Issues for Disability Weight Studies