J Breast Cancer.
2009 Mar;12(1):47-53. 10.4048/jbc.2009.12.1.47.
Clinical Analysis of Medullary Carcinoma of the Breast
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. bwpark@yumc.yonsei.ac.kr
- 2Department of Pathology, Yonsei University College of Medicine, Seoul, Korea.
- 3Brain Korea 21 Project, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2286579
- DOI: http://doi.org/10.4048/jbc.2009.12.1.47
Abstract
-
PURPOSE: Medullary carcinoma of the breast is a variant of breast cancer characterized by the histologic appearance of poorly differentiated cells surrounded by a prominent lymphoid stroma. Medullary carcinoma has been reported to carry a prognosis better than other invasive breast carcinomas, but it is frequently overdiagnosed due to the difficulty in diagnosis. The aim of this study was to assess the clinical manifestations and outcome of medullary carcinoma of the breast.
METHODS
We reviewed the data of 91 patients diagnosed with medullary carcinoma and 3,743 patients with invasive ductal carcinoma, not otherwise specified (NOS) from January 1980 to December 2005 at Yonsei University Severance Hospital. The clinicopathologic features, disease free survival (DFS) and overall survival (OS) for patients with medullary carcinoma were compared with those of the NOS patients.
RESULTS
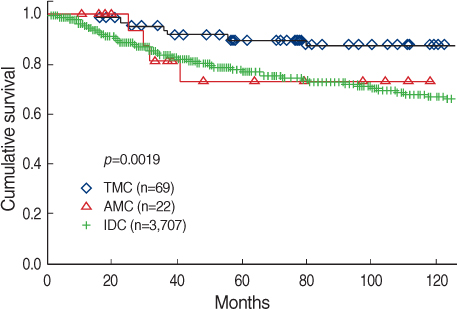
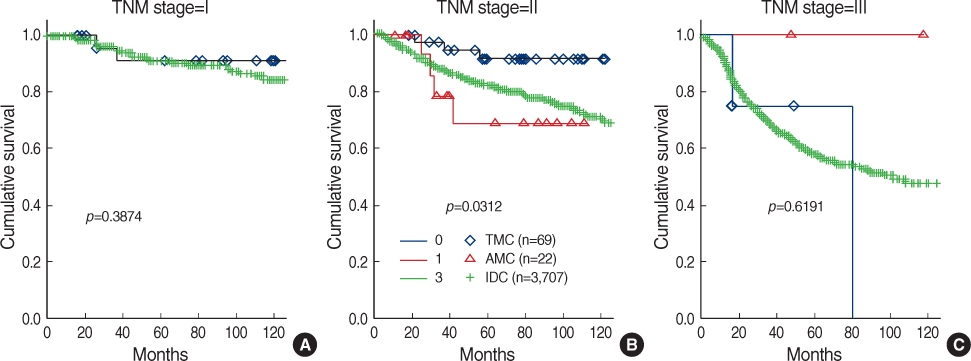
With reviewing the pathologic slides, 69 (75.8%) patients had findings compatible with typical medullary carcinoma (TMC) and the remaining 22 (24.2%) patients were reclassified as atypical medullary carcinoma (AMC). Early stage cancer was more frequent at medullary carcinoma and lymph node positive cancer was less frequent at medullary carcinoma. The expression of ER/PR was positive in either the TMC (18.9%/16.2%) and AMC (15.0%/20.0%) as compared to the NOS (63.2%/57.2%), and the difference was significant (p<0.001). In contrast, the HER-2/neu expression rate was significantly higher in the TMC (47.4%) and AMC (45.5%) than in the NOS (28.3%, p=0.001). The 10-year disease free survival and 10-year overall survival of the atypical medullary carcinoma patients (67.8%, 77.8%) were in fact similar to the NOS carcinoma patients (68.3%, 74.7%). There was significant difference in 10-year disease free survival and 10-year overall survival between the TMC (77.8%, 86.0%) and NOS carcinoma (68.3%, 74.7%) patients (p=0.002, p=0.006).
CONCLUSION
The clinical outcome of typical medullary carcinoma is favorable in spite of its aggressive pathologic features and it differs from atypical medullary carcinoma. For precise prediction of prognosis of medullary cancer, we should apply strict criteria for the diagnosis of subtype with medullary features.
MeSH Terms
Figure
Cited by 1 articles
-
Comparison of the Characteristics of Medullary Breast Carcinoma and Invasive Ductal Carcinoma
Inhye Park, Jiyoung Kim, Minkuk Kim, Soo Youn Bae, Se Kyung Lee, Won Ho Kil, Jeong Eon Lee, Seok Jin Nam
J Breast Cancer. 2013;16(4):417-425. doi: 10.4048/jbc.2013.16.4.417.
Reference
-
1. Moore OS, Foote FW Jr. The relatively favorable prognosis of medullary carcinoma of the breast. Cancer. 1949. 2:635–642.
Article2. Dardick I, Yazdi HM, Brosko C, Rippstein P, Hickey NM. A quantitative comparison of light and electron microscopic diagnoses in specimens obtained by fine-needle aspiration biopsy. Ultrastruct Pathol. 1991. 15:105–129.
Article3. Ridolfi RL, Rosen PP, Port A, Kinne D, Mike V. Medullary carcinoma of the breast: a clinicopathologic study with 10 year follow-up. Cancer. 1977. 40:1365–1385.
Article4. Ponsky JL, Gliga L, Reynolds S. Medullary carcinoma of the breast: an association with negative hormonal receptors. J Surg Oncol. 1984. 25:76–78.
Article5. Jensen ML, Kiaer H, Andersen J, Jensen V, Melsen F. Prognostic comparison of three classifications for medullary carcinomas of the breast. Histopathology. 1997. 30:523–532.
Article6. Tavassoli FA. Schnitt ST, editor. Infiltrating carcinomas, common and familiar special types: medullary carcinoma. Pathology the breast. 1992. Norwalk: Appleton & Lange;333–339.7. Fisher ER, Kenny JP, Sass R, Dimitrov NV, Siderits RH, Fisher B. Medullary cancer of the breast revisited. Breast Cancer Res Treat. 1990. 16:215–229.
Article8. Ellis IO, Galea M, Broughton N, Locker A, Blamey RW, Elston CW. Pathological prognostic factors in breast cancer. II. Histological type. Relationship with survival in a large study with long-term follow-up. Histopathology. 1992. 20:479–489.
Article9. Pedersen L, Zedeler K, Holck S, Schiodt T, Mouridsen HT. Medullary carcinoma of the breast, proposal for a new simplified histopathological definition. Based on prognostic observations and observations on inter- and intraobserver variability of 11 histopathological characteristics in 131 breast carcinomas with medullary features. Br J Cancer. 1991. 63:591–595.
Article10. Rapin V, Contesso G, Mouriesse H, Bertin F, Lacombe MJ, Piekarski JD, et al. Medullary breast carcinoma. A reevaluation of 95 cases of breast cancer with inflammatory stroma. Cancer. 1988. 61:2503–2510.
Article11. Fisher ER, Gregorio RM, Fisher B, Redmond C, Vellios F, Sommers SC. The pathology of invasive breast cancer. A syllabus derived from findings of the National Surgical Adjuvant Breast Project (protocol no. 4). Cancer. 1975. 36:1–85.
Article12. Pedersen L, Holck S, Schiodt T, Zedeler K, Mouridsen HT. Inter- and intraobserver variability in the histopathological diagnosis of medullary carcinoma of the breast, and its prognostic implications. Breast Cancer Res Treat. 1989. 14:91–99.
Article13. Pedersen L, Holck S, Schiodt T, Zedeler K, Mouridsen HT. Medullary carcinoma of the breast, prognostic importance of characteristic histopathological features evaluated in a multivariate Cox analysis. Eur J Cancer. 1994. 30A:1792–1797.
Article14. Wargotz ES, Silverberg SG. Medullary carcinoma of the breast: a clinicopathologic study with appraisal of current diagnostic criteria. Hum Pathol. 1988. 19:1340–1346.
Article15. Rubens JR, Lewandrowski KB, Kopans DB, Koerner FC, Hall DA, McCarthy KA. Medullary carcinoma of the breast. Overdiagnosis of a prognostically favorable neoplasm. Arch Surg. 1990. 125:601–604.16. Black CL, Morris DM, Goldman LI, McDonald JC. The significance of lymph node involvement in patients with medullary carcinoma of the breast. Surg Gynecol Obstet. 1983. 157:497–499.17. Fourquet A, Vilcoq JR, Zafrani B, Schlienger P, Jullien D, Campana F. Medullary breast carcinoma: the role of radiotherapy as primary treatment. Radiother Oncol. 1987. 10:1–6.
Article18. Reinfuss M, Stelmach A, Mitus J, Rys J, Duda K. Typical medullary carcinoma of the breast: a clinical and pathological analysis of 52 cases. J Surg Oncol. 1995. 60:89–94.
Article19. Jensen ML, Kiaer H, Melsen F. Medullary breast carcinoma vs. poorly differentiated ductal carcinoma: an immunohistochemical study with keratin 19 and oestrogen receptor staining. Histopathology. 1996. 29:241–245.
Article20. Xu R, Feiner H, Li P, Yee H, Inghirami G, Delgado Y, et al. Differential amplification and overexpression of HER-2/neu, p53, MIB1, and estrogen receptor/progesterone receptor among medullary carcinoma, atypical medullary carcinoma, and high-grade invasive ductal carcinoma of breast. Arch Pathol Lab Med. 2003. 127:1458–1464.
Article21. Jacquemier J, Padovani L, Rabayrol L, Lakhani SR, Penault-Llorca F, Denoux Y, et al. Typical medullary breast carcinomas have a basal/myoepithelial phenotype. J Pathol. 2005. 207:260–268.
Article22. Kurtz JM, Jacquemier J, Torhorst J, Spitalier JM, Amalric R, Hunig R, et al. Conservation therapy for breast cancers other than infiltrating ductal carcinoma. Cancer. 1989. 63:1630–1635.
Article23. Kim SW, Kang HJ, Noh DY, Youn YK, Oh SK, Choe KJ. Comparison of the prognostic factors between medullary cancer and infiltrating ductal carcinoma in the breast. J Korean Surg Soc. 2000. 59:182–190.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fine Needle Aspiration Cytology of Medullary Carcinoma of the Breast: A Case Report
- Medullary carcinoma of the breast: Imaging findings characteristics vs histologic classification
- Reclassification of the Medullary Carcinoma and It's Clinical Characteristics
- Metastatic Medullary Carcinoma of Thyroid to Breast; A Case Initially Diagnosed as Primary Invasive Lobular Carcinoma: A Case Report
- Huge Exophytic Atypical Medullary Breast Cancer