J Breast Cancer.
2010 Mar;13(1):31-36. 10.4048/jbc.2010.13.1.31.
Clinicopathologic Review of the Intraductal Papilloma of Breast
- Affiliations
-
- 1Department of Surgery, Konyang University Hospital, Daejeon, Korea. dsyoonmd@kyuh.ac.kr
- 2Department of Pathology, Konyang University Hospital, Daejeon, Korea.
- 3Department of Radiology, Konyang University Hospital, Daejeon, Korea.
- 4Department of Pathology, St. Mary's Hospital, Daejeon, Korea.
- 5Park's Breast Clinic, Daejeon, Korea.
- KMID: 2286557
- DOI: http://doi.org/10.4048/jbc.2010.13.1.31
Abstract
- PURPOSE
Intraductal papilloma of the breast (IDP) is the most common causes of nipple discharge and it is often a solitary, centrally located tumor that most commonly occurs in the fifth and sixth decades of life. There have been many conflicting reports on the malignant potential of IDP.
METHODS
From February 2003 to November 2008, we operated 161 patients who were diagnosed with IDP at Konyang University Hospital. A retrospective review of all the pathologic reports and the corresponding radiological reports was undertaken.
RESULTS
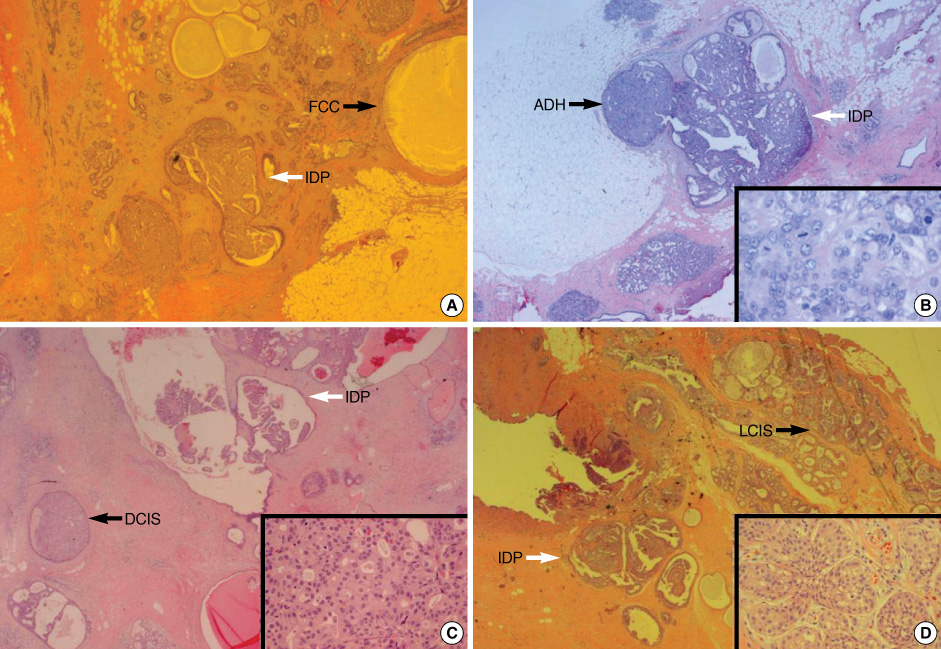
The mean age of the patients was 43.23 years (SD, +/-10.1). Eighty-three (51.6%) had nipple discharge, 37 (44.6%) had bloody discharge and 46 (55.4%) had yellowish serous discharge. Twenty-four had a mass and 2 had both bloody discharge and a mass. Radiologic significant findings were shown on 20 mammography exams, 71 ductography exams and 157 breast ultrasound exams. Onehundred forty-four (89.4%) patients with IDP or papillomatosis had surrounding pathologic lesions in the operated specimen according to the final pathology, 107 (66.5%) had fibrocystic change, 26 (16.1%) had fibroadenoma, 30 (18.6%) had atypical ductal hyperplasia (ADH), 11 (6.8%) had carcinoma in situ and 4 (2.5%) had invasive ductal carcinoma. During the follow up, 7 patients (4.3%) developed recurrent IDP, 3 patients developed ADH and 5 patients developed carcinoma in situ (4 patients had ductal carcinoma in situ and 1 patient had lobular carcinoma in situ).
CONCLUSION
Intraductal papilloma should be closely followed up due to its malignant potential and the surrounding breast tissue with IDP should be carefully evaluated due to the high rate of developing other precancerous lesions.
Keyword
MeSH Terms
Figure
Reference
-
1. Korean Breast Cancer Society. The breast. 2005. 2nd ed. Seoul: Ilchokak.2. Macgrogan G, Moinnfar F, Raju U. Tavassoli FA, Devilee PD, editors. Intraductal papillary neoplasm. Pathology and Genetics: Tumours of the Breast. 2003. Lyon: IARC Press;76–80.3. Park JH, Bae JS, Suh YJ, Park WC, Song BJ, Kim JS, et al. Clinicopathologic features of the papillary breast lesions diagnosed on ultrasonography-guided core needle biopsy. J Breast Cancer. 2007. 10:269–272.
Article4. Hwang JS. Correlation of Intraductal papilloma and their malignant tansformation and treatment of intraductal papilloma. J Korean Surg Soc. 1962. 4:53.5. Nelson RS, Hoehn JL. Twenty-year outcome following central duct resection for bloody nipple discharge. Ann Surg. 2006. 243:522–524.
Article6. Lamont JP, Dultz RP, Kuhn JA, Grant MD, Jones RC. Galactography in patients with nipple discharge. Proc (Bayl Univ Med Cent). 2000. 13:214–216.
Article7. Park YL, Shin JH, Pae WK. Dye-injection microdochectomy for intraductal papilloma of the breast. J Korean Surg Soc. 1999. 56:486–490.8. Gioffré Florio MA, Famá F, Giacobbe G, Pollicino A, Scarfò P. Nipple discharge: personal experience with 2,818 cases. Chir Ital. 2003. 55:357–364.9. Mulligan AM, O'Malley FP. Papillary lesions of the breast: a review. Adv Anat Pathol. 2007. 14:108–119.10. Page DL, Salhany KE, Jensen RA, Dupont WD. Subsequent breast carcinoma risk after biopsy with atypia in a breast papilloma. Cancer. 1996. 15:258–266.
Article11. Agoff SN, Lawton TJ. Papillary lesions of the breast with and without atypical ductal hyperplasia: can we accurately predict benign behavior from core needle biopsy? Am J Clin Pathol. 2004. 122:440–443.
Article12. Sohn V, Keylock J, Arthurs Z, Wilson A, Herbert G, Perry J, et al. Breast papillomas in the era of the percutaneous needle biopsy. Ann Surg Oncol. 2007. 14:2979–2984.
Article13. Matsunaga T, Kawakami Y, Namba K, Fujii M. Intraductal biopsy for diagnosis and treatment of intraductal lesions of the breast. Cancer. 2004. 101:2164–2169.
Article14. Ciatto S, Andreoli C, Cirillo A, Bonardi R, Bianchi S, Santoro G, et al. The risk of breast cancer subsequent to histologic diagnosis of benign intraductal papilloma follow-up study of 339 cases. Tumori. 1991. 77:41–43.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Dye-injection Microdochectomy for Intraductal Papilloma of the Breast
- A Case Report of Intraductal Papilloma in a Young Female Patient with Bloody Nipple Discharge
- Clinicopathologic Features of the Papillary Breast Lesions Diagnosed on Ultrasonography-guided Core Needle Biopsy
- A Case of Intraductal Papilloma arising in the Parotid Gland
- Intraductal Papilloma Arising in the Sublingual Salivary Gland