J Breast Cancer.
2012 Mar;15(1):128-132. 10.4048/jbc.2012.15.1.128.
A Case Report of Breast Cancer with Extensive Pulmonary Lymphovascular Tumor Emboli
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea. kyunghunlee@snu.ac.kr
- 2Department of Pathology, Seoul National University Hospital, Seoul, Korea.
- 3Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Thoracic Surgery, Seoul National University Hospital, Seoul, Korea.
- KMID: 2286485
- DOI: http://doi.org/10.4048/jbc.2012.15.1.128
Abstract
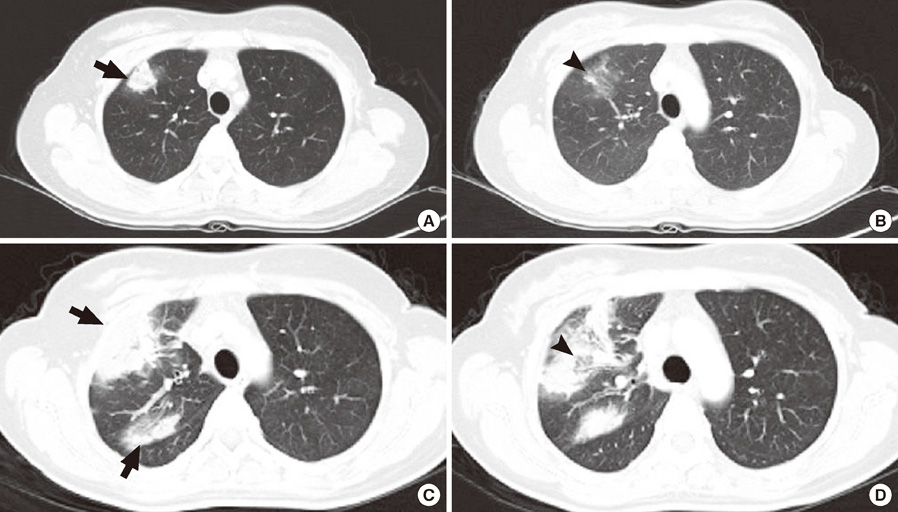
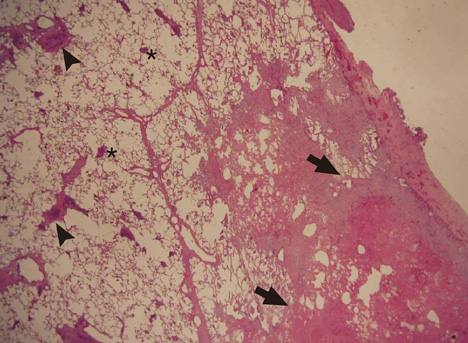
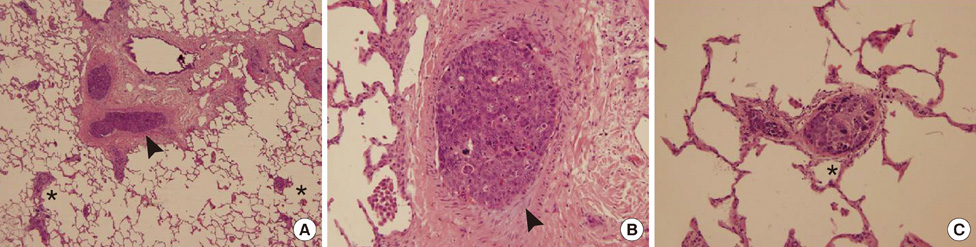
- We describe a patient with breast cancer who relapsed with an extensive pulmonary lymphovascular tumor embolism. A 38-year-old female, who previously received neoadjuvant chemotherapy and curative resection of breast cancer, underwent adjuvant chemotherapy and was referred to the emergency room because of sudden-onset pleuritic chest pain lasting for 10 days. Despite a trial of empirical antibiotics, the chest pain and the extent of consolidative lung lesion on chest radiographs rapidly aggravated. We performed an open lung biopsy to confirm the etiology. The histopathological review revealed a hemorrhagic infarction caused by lymphovascular tumor emboli from a metastatic breast carcinoma. Palliative first-line chemotherapy was administered, consisting of ixabepilone and capecitabine, and the lung lesion improved markedly.
Keyword
MeSH Terms
Figure
Reference
-
1. Goldhaber SZ, Dricker E, Buring JE, Eberlein K, Godleski JJ, Mayer RJ, et al. Clinical suspicion of autopsy-proven thrombotic and tumor pulmonary embolism in cancer patients. Am Heart J. 1987. 114:1432–1435.
Article2. Roberts KE, Hamele-Bena D, Saqi A, Stein CA, Cole RP. Pulmonary tumor embolism: a review of the literature. Am J Med. 2003. 115:228–232.
Article3. Sostman HD, Brown M, Toole A, Bobrow S, Gottschalk A. Perfusion scan in pulmonary vascular/lymphangitic carcinomatosis: the segmental contour pattern. AJR Am J Roentgenol. 1981. 137:1072–1074.
Article4. Gajdos C, Nierman DM, Moqtaderi FF, Brower ST, Lento P, Bleiweiss IJ. Microscopic pulmonary tumor emboli: an unusual presentation of breast cancer. Breast J. 2000. 6:273–275.
Article5. Bassiri AG, Haghighi B, Doyle RL, Berry GJ, Rizk NW. Pulmonary tumor embolism. Am J Respir Crit Care Med. 1997. 155:2089–2095.
Article6. Aiyappan V, Alwail A. Pulmonary tumor thromboembolism: a case report and review of literature. Ann Thorac Med. 2007. 2:169–170.
Article7. Ejlertsen B, Jensen MB, Rank F, Rasmussen BB, Christiansen P, Kroman N, et al. Population-based study of peritumoral lymphovascular invasion and outcome among patients with operable breast cancer. J Natl Cancer Inst. 2009. 101:729–735.
Article8. Kawasaki H, Ogura H, Arai Y, Baba S, Kosugi I, Tsutsui Y, et al. Aggressive progression of breast cancer with microscopic pulmonary emboli possessing a stem cell-like phenotype independent of its origin. Pathol Int. 2010. 60:228–234.
Article9. Thomas ES, Gomez HL, Li RK, Chung HC, Fein LE, Chan VF, et al. Ixabepilone plus capecitabine for metastatic breast cancer progressing after anthracycline and taxane treatment. J Clin Oncol. 2007. 25:5210–5217.
Article10. Perez EA, Patel T, Moreno-Aspitia A. Efficacy of ixabepilone in ER/PR/HER2-negative (triple-negative) breast cancer. Breast Cancer Res Treat. 2010. 121:261–271.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Angiomatoid Spitz Nevus with High Cellularity and Lymphovascular Tumor Emboli-like Features
- A Case of Locally Advanced Breast Cancer Complicated by Pulmonary Tumor Thrombotic Microangiopathy
- A Case of Multiple Right Atrial Myxomas with Pulmonary Embolism
- Predictive Factors Affecting Axillary Lymph Node Metastasis in Patients with Invasive Breast Carcinoma of 1 cm or Less
- Primary testicular carcinoid tumor with marked lymphovascular invasion