Ewha Med J.
2013 Mar;36(1):51-57. 10.12771/emj.2013.36.1.51.
Clinical Relevance of EGFR Mutations in Colorectal Cancer Patients
- Affiliations
-
- 1Department of Surgery, Ewha Womans University School of Medicine, Seoul, Korea. eastgate@ewha.ac.kr
- KMID: 2284015
- DOI: http://doi.org/10.12771/emj.2013.36.1.51
Abstract
OBJECTIVES
The EGFR plays an important role in tumorigenesis and tumor progression of colorectal cancer, and leads to the activation of intracellular signaling pathways. The use of anti-EGFR-targeted therapy has increased for patients with colorectal cancer, but patients with EGFR mutations will be resistant to anti-EGFR-targeted therapy. The identification of gene mutations is critical in cancer treatment; therefore, the aim of this study is to investigate the incidences of EGFR mutations in colorectal cancer patients in Korea.
METHODS
We reviewed 58 colorectal cancer patients who underwent operations between 2003 and 2006, retrospectively. We analyzed their EGFR mutations in 4 loci by DNA sequencing. In addition, we analyzed the correlation between the presence of EGFR mutation and patients' clinicopathologic features.
RESULTS
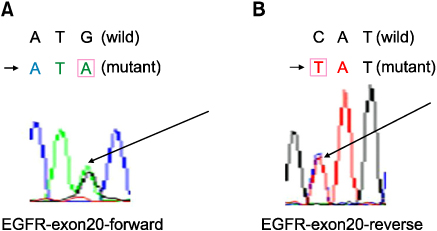
Of the 58 patients, 35 patients were male and 23 were female. Their mean age was 63.28+/-11.18 years. Two patients (3.45%) were diagnosed as stage Tis, 7 patients (12.07%) had stage I, 24 patients (41.38%) had stage II, 20 patients (34.48%) had stage III, and 5 patients (8.62%) had stage IV. As a result of mutational analysis, EGFR mutations on exon 20 were detected in 13 patients (22.41%, G-->A transitions). EGFR mutations on exon 18, 19 and 21 were not detected. EGFR mutation increased in the earlier stage and the absence of lymph node metastasis (P=0.028).
CONCLUSION
The incidence of EGFR mutation in Korean colorectal cancer patients is 22.41%. In addition, EGFR mutation significantly increased in the earlier stage and the absence of lymph node metastasis.
Keyword
MeSH Terms
Figure
Reference
-
1. de Castro-Carpeño J, Belda-Iniesta C, Casado Sáenz E, Hernández Agudo E, Feliu Batle J, González Barón M. EGFR and colon cancer: a clinical view. Clin Transl Oncol. 2008. 10:6–13.2. Ponz-Sarvisé M, Rodríguez J, Viudez A, Chopitea A, Calvo A, García-Foncillas J, et al. Epidermal growth factor receptor inhibitors in colorectal cancer treatment: What's new? World J Gastroenterol. 2007. 13:5877–5887.3. Sameer AS, Chowdhri NA, Abdullah S, Shah ZA, Siddiqi MA. Mutation pattern of K-ras gene in colorectal cancer patients of Kashmir: a report. Indian J Cancer. 2009. 46:219–225.4. Yun SH. Molecular targeted therapy in colorectal cancer. J Korean Soc Coloproctol. 2004. 20:180–188.5. Kim HA, Lee RA, Hwang DY, Park SH. The significances of EGFR overexpression in colorectal cancer. J Korean Soc Coloproctol. 2005. 21:36–41.6. Jang TW, Oak CH, Chang HK, Suo SJ, Jung MH. EGFR and KRAS mutations in patients with adenocarcinoma of the lung. Korean J Intern Med. 2009. 24:48–54.7. Hynes NE, Lane HA. ERBB receptors and cancer: the complexity of targeted inhibitors. Nat Rev Cancer. 2005. 5:341–354.8. Carpenter G, Cohen S. Epidermal growth factor. J Biol Chem. 1990. 265:7709–7712.9. Zhou Y, Li S, Hu YP, Wang J, Hauser J, Conway AN, et al. Blockade of EGFR and ErbB2 by the novel dual EGFR and ErbB2 tyrosine kinase inhibitor GW572016 sensitizes human colon carcinoma GEO cells to apoptosis. Cancer Res. 2006. 66:404–411.10. Kim ES, Khuri FR, Herbst RS. Epidermal growth factor receptor biology (IMC-C225). Curr Opin Oncol. 2001. 13:506–513.11. McKay JA, Murray LJ, Curran S, Ross VG, Clark C, et al. Evaluation of the epidermal growth factor receptor (EGFR) in colorectal tumours and lymph node metastases. Eur J Cancer. 2002. 38:2258–2264.12. Di Fiore F, Blanchard F, Charbonnier F, Le Pessot F, Lamy A, Galais MP, et al. Clinical relevance of KRAS mutation detection in metastatic colorectal cancer treated by Cetuximab plus chemotherapy. Br J Cancer. 2007. 96:1166–1169.13. Nagahara H, Mimori K, Ohta M, Utsunomiya T, Inoue H, Barnard GF, et al. Somatic mutations of epidermal growth factor receptor in colorectal carcinoma. Clin Cancer Res. 2005. 11:1368–1371.14. Kalikaki A, Koutsopoulos A, Trypaki M, Souglakos J, Stathopoulos E, Georgoulias V, et al. Comparison of EGFR and K-RAS gene status between primary tumours and corresponding metastases in NSCLC. Br J Cancer. 2008. 99:923–929.15. Park SH, Ha SY, Lee JI, Lee H, Sim H, Kim YS, et al. Epidermal growth factor receptor mutations and the clinical outcome in male smokers with squamous cell carcinoma of lung. J Korean Med Sci. 2009. 24:448–452.16. Barber TD, Vogelstein B, Kinzler KW, Velculescu VE. Somatic mutations of EGFR in colorectal cancers and glioblastomas. N Engl J Med. 2004. 351:2883.17. Ogino S, Meyerhardt JA, Cantor M, Brahmandam M, Clark JW, Namgyal C, et al. Molecular alterations in tumors and response to combination chemotherapy with gefitinib for advanced colorectal cancer. Clin Cancer Res. 2005. 11:6650–6656.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidermal Growth Factor Receptor Mutations in Colorectal Cancer Patients
- EGFR Tyrosine Kinase Inhibitors for NSCLC
- Chronicles of EGFR Tyrosine Kinase Inhibitors: Targeting EGFR C797S Containing Triple Mutations
- A Case of Patient with Lung Adenocarcinoma with Double Rare EGFR Mutation of G719C and L861Q
- Are Mutations of the EGFR Gene Promising Predictive Markers for Anti-EGFR mAbs in Colorectal Carcinomas?