Ewha Med J.
2012 Sep;35(2):135-139. 10.12771/emj.2012.35.2.135.
Long Term Improvement of Dysphagia in Lateral Medullary Infarction: A Case Report
- Affiliations
-
- 1Department of Rehabilitation Medicine, Ewha Womans University School of Medicine, Seoul, Korea. ocrystal@ewha.ac.kr
- 2Department of Neurosurgery, Ewha Womans University School of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Ewha Womans University School of Medicine, Seoul, Korea.
- KMID: 2284006
- DOI: http://doi.org/10.12771/emj.2012.35.2.135
Abstract
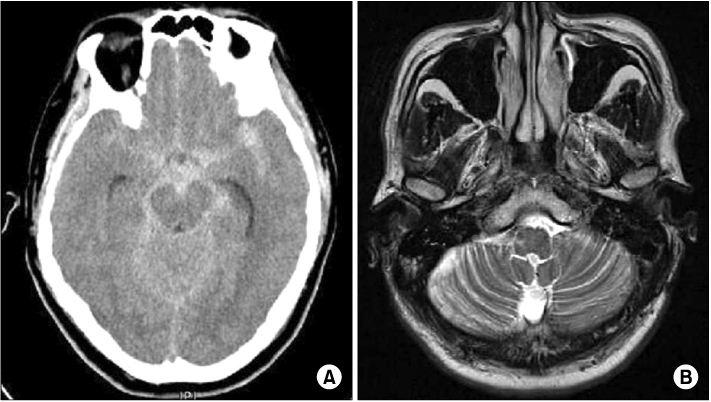
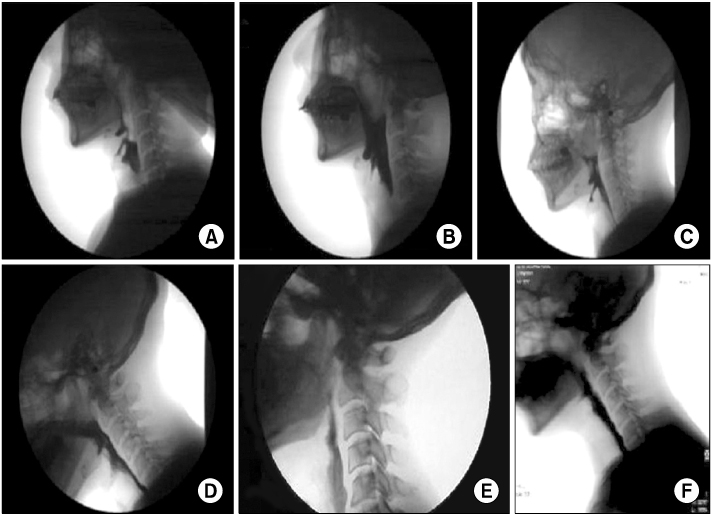
- This report concerns a male patient suffered from refractory dysphagia after subarachnoid hemorrhage. A 49-year-old man admitted with severe headache followed by mental change. Imaging studies revealed that subarachnoid hemorrhage was located in basal cistern, and demonstrated ruptured vertebral dissecting aneurysm. After operation, the patient recovered well except severe dysphagia. Initial VFSS showed aspiration in fluid trial, penetration in semisolid bolus, and large amount of pharyngeal residue with poor relaxation of upper esophageal sphincter. For about 5 months, his symptom and several follow-up VFSS findings did not show marked improvement by various treatments. On magnetic resonance imaging for further evaluation of his brain lesion, an old infarction in right lateral side of medulla was found. He kept dysphagia rehabilitation more than one year, and his symptom improved to the level of oral feeding at last.
MeSH Terms
Figure
Reference
-
1. Perlman AL. Dysphagia in stroke patients. Semin Neurol. 1996. 16:341–348.2. Daniels SK, Brailey K, Priestly DH, Herrington LR, Weisberg LA, Foundas AL. Aspiration in patients with acute stroke. Arch Phys Med Rehabil. 1998. 79:14–19.3. Hamdy S, Mikulis DJ, Crawley A, Xue S, Lau H, Henry S, et al. Cortical activation during human volitional swallowing: an event-related fMRI study. Am J Physiol. 1999. 277(1 Pt 1):G219–G225.4. Zald DH, Pardo JV. The functional neuroanatomy of voluntary swallowing. Ann Neurol. 1999. 46:281–286.5. Langmore SE, Miller RM. Behavioral treatment for adults with oropharyngeal dysphagia. Arch Phys Med Rehabil. 1994. 75:1154–1160.6. Park YJ, Yang HS, Cha DY. Neuromuscular electrical stimulation therapy for patients with chronic dysphagia caused by stroke. J Korean Acad Rehabil Med. 2007. 31:636–641.7. Shaw GY, Sechtem PR, Searl J, Keller K, Rawi TA, Dowdy E. Transcutaneous neuromuscular electrical stimulation (VitalStim) curative therapy for severe dysphagia: myth or reality? Ann Otol Rhinol Laryngol. 2007. 116:36–44.8. Lee CK, Kim JA. Pattern of post-stroke swallowing disorder according to the brain lesion. J Korean Acad Rehabil Med. 2001. 25:193–201.9. Ahsan SF, Meleca RJ, Dworkin JP. Botulinum toxin injection of the cricopharyngeus muscle for the treatment of dysphagia. Otolaryngol Head Neck Surg. 2000. 122:691–695.10. Han TR, Kim JH, Kim HS, Paik NJ. Functional outcomes of subarachnoid hemorrhage and other stroke. J Korean Acad Rehabil Med. 1992. 16:139–146.11. Murakami K, Takahashi N, Matsumura N, Umezawa K, Midorikawa H, Nishijima M. Vertebrobasilar artery dissection presenting with simultaneous subarachnoid hemorrhage and brain stem infarction: case report. Surg Neurol. 2003. 59:18–22.12. Bian RX, Choi IS, Kim JH, Han JY, Lee SG. Impaired opening of the upper esophageal sphincter in patients with medullary infarctions. Dysphagia. 2009. 24:238–245.13. Prosiegel M, Holing R, Heintze M, Wagner-Sonntag E, Wiseman K. Swallowing therapy: a prospective study on patients with neurogenic dysphagia due to unilateral paresis of the vagal nerve, Avellis' syndrome, Wallenberg's syndrome, posterior fossa tumours and cerebellar hemorrhage. Acta Neurochir Suppl. 2005. 93:35–37.14. Foley N, Teasell R, Salter K, Kruger E, Martino R. Dysphagia treatment post stroke: a systematic review of randomised controlled trials. Age Ageing. 2008. 37:258–264.15. Aydogdu I, Ertekin C, Tarlaci S, Turman B, Kiylioglu N, Secil Y. Dysphagia in lateral medullary infarction (Wallenberg's syndrome): an acute disconnection syndrome in premotor neurons related to swallowing activity? Stroke. 2001. 32:2081–2087.16. Park YJ, Yang HS, Cha DY. Neuromuscular electrical stimulation therapy for patients with chronic dysphagia caused by stroke. J Korean Acad Rehabil Med. 2007. 31:636–641.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Isolated Axial Lateropulsion in Lateral Medullary Infarction
- A Case Of Lateral Medullary Infarction Presenting as Isolated Dysphagia with Unilateral Vocal Fold Paralysis
- Isolated Dysphagia Caused by Failure of Cricopharyngeal Muscle Relaxation after Left Lateral Medullary Lacunar Infarction: A case report
- Pure Limb Ataxia as Isolated Manifestation in Lateral Medullary Infarction
- A Case of Lateral Medullary Syndrome with Ipsilesional Nystagmus due to Intramedullary Hemorrhage