Current Status of Glycemic Control of Patients with Diabetes in Korea: The Fifth Korea National Health and Nutrition Examination Survey
- Affiliations
-
- 1Department of Endocrinology and Metabolism, Ajou University School of Medicine, Suwon, Korea.
- 2Division of Endocrinology and Metabolism, Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 4Division of Endocrinology and Metabolism, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea.
- 5Division of Endocrinology and Metabolism, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea.
- 6Department of Internal Medicine, Mitochondrial Research Group, Inje University Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- 7Division of Endocrinology and Metabolism, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 8Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea. skh2k@kuh.ac.kr
- KMID: 2280690
- DOI: http://doi.org/10.4093/dmj.2014.38.3.197
Abstract
- BACKGROUND
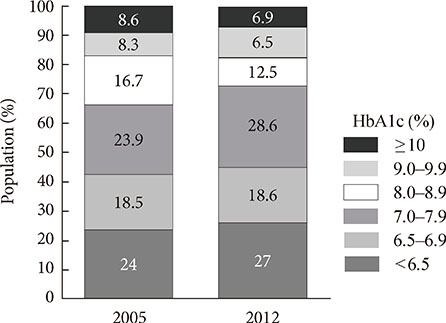
The Korea National Health and Nutrition Examination Survey (KNHANES) III (2005) reported that 22.9% of individuals with diabetes have a glycated hemoglobin (HbA1c) <6.5% and that 43.5% have an HbA1c <7%. We investigated the levels of glycemic control and the factors associated with glycemic control using data from the KNHANES V (2010 to 2012).
METHODS
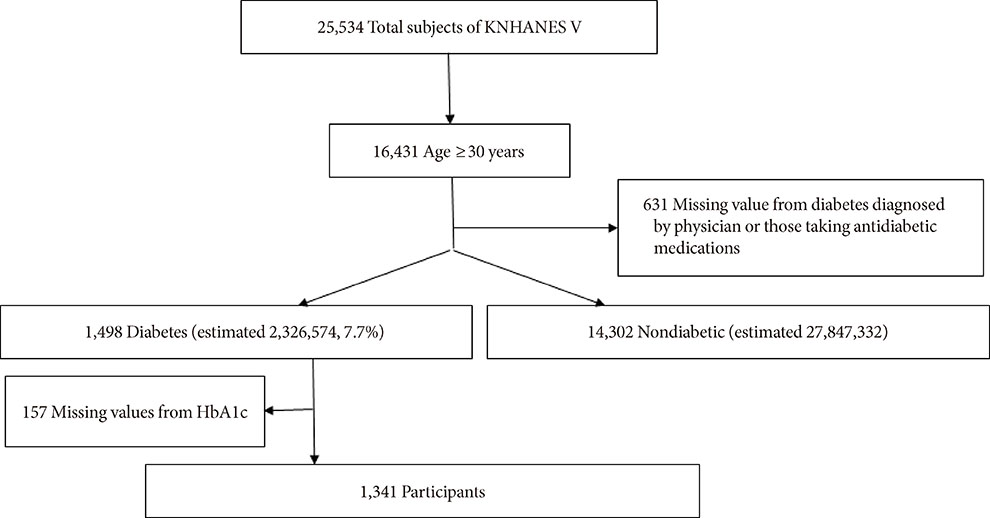
Subjects with diabetes diagnosed by a physician or those taking antidiabetic medications were classified as individuals with known diabetes. Of 1,498 subjects aged > or =30 years with diabetes, we excluded 157 individuals who were missing HbA1c data. A total of 1,341 subjects were included in the final analysis.
RESULTS
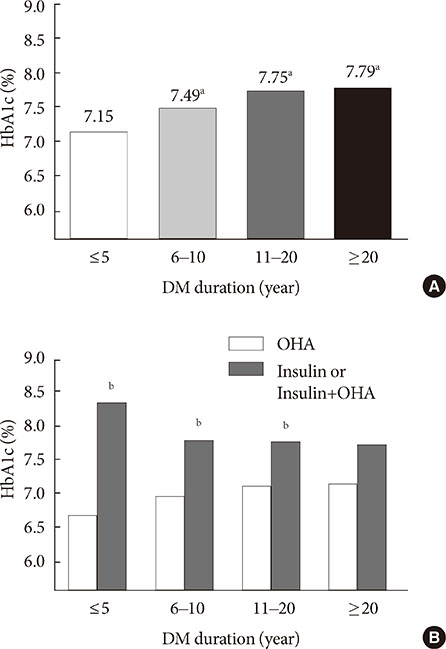
The prevalence of known diabetes was 7.7% (n=1,498, estimated to be 2.32 million people). The proportions of well-controlled diabetes meeting a HbA1c goal of <6.5% and <7% were 27% and 45.6%, respectively. HbA1c increased as the duration of diabetes increased. HbA1c in subjects with a duration of diabetes < or =5 years was lower than in subjects with a duration >5 years. HbA1c in the group taking only oral hypoglycemic agents (OHAs) was significantly lower than that in the group administered only insulin or OHA and insulin in combination. In logistic regression analysis, a longer duration of diabetes, insulin use and the absence of chronic renal failure were associated with HbA1c levels >6.5%.
CONCLUSION
The level of adequate glycemic control was similar to but slightly improved compared with previous levels. The glycemic control of long-standing diabetes patients is more difficult even though they receive insulin treatment.
Keyword
MeSH Terms
Figure
Cited by 10 articles
-
Trends in metabolic risk factors among patients with diabetes mellitus according to income levels: the Korea National Health and Nutrition Examination Surveys 1998 ~ 2014
Sukyung Cho, Kyong Park
J Nutr Health. 2019;52(2):206-216. doi: 10.4163/jnh.2019.52.2.206.Ten-Year Mortality Trends for Adults with and without Diabetes Mellitus in South Korea, 2003 to 2013
Kyeong Jin Kim, Tae Yeon Kwon, Sungwook Yu, Ji A Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Dong Seop Choi, Sin Gon Kim, Yousung Park, Nam Hoon Kim
Diabetes Metab J. 2018;42(5):394-401. doi: 10.4093/dmj.2017.0088.Past and Current Status of Adult Type 2 Diabetes Mellitus Management in Korea: A National Health Insurance Service Database Analysis
Seung-Hyun Ko, Kyungdo Han, Yong-ho Lee, Junghyun Noh, Cheol-Young Park, Dae-Jung Kim, Chang Hee Jung, Ki-Up Lee, Kyung-Soo Ko,
Diabetes Metab J. 2018;42(2):93-100. doi: 10.4093/dmj.2018.42.2.93.Diabetes Fact Sheets in Korea, 2018: An Appraisal of Current Status
Bo-Yeon Kim, Jong Chul Won, Jae Hyuk Lee, Hun-Sung Kim, Jung Hwan Park, Kyoung Hwa Ha, Kyu Chang Won, Dae Jung Kim, Kyong Soo Park
Diabetes Metab J. 2019;43(4):487-494. doi: 10.4093/dmj.2019.0067.Diabetes in Asians
Eun-Jung Rhee
Endocrinol Metab. 2015;30(3):263-269. doi: 10.3803/EnM.2015.30.3.263.The Side Effects of Sodium Glucose Cotransporter 2 (SGLT2) Inhibitor
Won Jin Kim, Sang Soo Kim
J Korean Diabetes. 2014;15(3):158-162. doi: 10.4093/jkd.2014.15.3.158.Inhibition of advanced glycation end product formation by burdock root extract
Darye Lee, Choon Young Kim
J Nutr Health. 2016;49(4):233-240. doi: 10.4163/jnh.2016.49.4.233.Association between Diabetes Education Status and Clinical Outcomes of Patients with Diabetes Mellitus: Analysis of the Fifth Korea National Health and Nutrition Examination Survey (KNHANES V)
Jun Sung Kwon, Won Jun Kim, Yang Hee Han, Hyun Joong Kim, Sa Young Shin, Kyoo Ho Choi, Jae Hyuck Jun, Myoung Sook Shim, Jin Yeob Kim
J Korean Diabetes. 2014;15(4):236-243. doi: 10.4093/jkd.2014.15.4.236.Factors Influencing Glycemic Control among Type 2 Diabetes Mellitus Patients: The Sixth Korea National Health and Nutrition Examination Survey (2013~2015)
Mee Ock Gu
Korean J Adult Nurs. 2019;31(3):235-248. doi: 10.7475/kjan.2019.31.3.235.A Position Statement on Diabetes with β-Cell Failure
Ji Yoon Kim, Sang-Man Jin, Gyuri Kim, Soo Kyoung Kim, Won Jun Kim, Sun Joon Moon, Jee Hee Yoo, Da Young Lee, Seung-Eun Lee, Ji Eun Jun, Jae Hyeon Kim
J Korean Diabetes. 2024;25(3):124-134. doi: 10.4093/jkd.2024.25.3.124.
Reference
-
1. Statistics Korea: Causes of death statistics 2012. updated 2013 Sep 25. Available from: http://kostat.go.kr.2. Nolan CJ, Damm P, Prentki M. Type 2 diabetes across generations: from pathophysiology to prevention and management. Lancet. 2011; 378:169–181.3. Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA. 2002; 287:2570–2581.4. Jeon JY, Ko SH, Kwon HS, Kim NH, Kim JH, Kim CS, Song KH, Won JC, Lim S, Choi SH, Jang MJ, Kim Y, Oh K, Kim DJ, Cha BY. Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association. Prevalence of diabetes and prediabetes according to fasting plasma glucose and HbA1c. Diabetes Metab J. 2013; 37:349–357.5. Choi YJ, Kim HC, Kim HM, Park SW, Kim J, Kim DJ. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998-2005. Diabetes Care. 2009; 32:2016–2020.6. Task Force Team for Basic Statistical Study of Korean Diabetes Mellitus of Korean Diabetes Association. Park IB, Kim J, Kim DJ, Chung CH, Oh JY, Park SW, Lee J, Choi KM, Min KW, Park JH, Son HS, Ahn CW, Kim H, Lee S, Lee IB, Choi I, Baik SH. Diabetes epidemics in Korea: reappraise nationwide survey of diabetes "diabetes in Korea 2007". Diabetes Metab J. 2013; 37:233–239.7. Ali MK, Bullard KM, Saaddine JB, Cowie CC, Imperatore G, Gregg EW. Achievement of goals in U.S. diabetes care, 1999-2010. N Engl J Med. 2013; 368:1613–1624.8. Nathan DM, Buse JB, Davidson MB, Heine RJ, Holman RR, Sherwin R, Zinman B. Professional Practice Committee American Diabetes Association. European Association for the Study of Diabetes. Management of hyperglycaemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy. A consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetologia. 2006; 49:1711–1721.9. Yu NC, Su HY, Chiou ST, Yeh MC, Yeh SW, Tzeng MS, Sheu WH. Trends of ABC control 2006-2011: a National Survey of Diabetes Health Promotion Institutes in Taiwan. Diabetes Res Clin Pract. 2013; 99:112–119.10. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998; 352:837–853.11. Wajchenberg BL. beta-cell failure in diabetes and preservation by clinical treatment. Endocr Rev. 2007; 28:187–218.12. Walter H, Lubben G. Potential role of oral thiazolidinedione therapy in preserving beta-cell function in type 2 diabetes mellitus. Drugs. 2005; 65:1–13.13. Cariou B, Charbonnel B, Staels B. Thiazolidinediones and PPARgamma agonists: time for a reassessment. Trends Endocrinol Metab. 2012; 23:205–215.14. Campbell JE, Drucker DJ. Pharmacology, physiology, and mechanisms of incretin hormone action. Cell Metab. 2013; 17:819–837.15. Drucker DJ, Sherman SI, Gorelick FS, Bergenstal RM, Sherwin RS, Buse JB. Incretin-based therapies for the treatment of type 2 diabetes: evaluation of the risks and benefits. Diabetes Care. 2010; 33:428–433.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intake of Fruit and Glycemic Control in Korean Patients with Diabetes Mellitus Using the Korea National Health and Nutrition Examination Survey
- Factors Associated with Poor Glycemic Control among Patients with Type 2 Diabetes Mellitus: The Fifth Korea National Health and Nutrition Examination Survey (2010-2012)
- Associations between grip strength and glycemic control in type 2 diabetes mellitus: an analysis of data from the 2014-2019 Korea National Health and Nutrition Examination Survey
- Diabetes-related Characteristics in Men with Diabetes for the Glucose Control Group and Noncontrol Group
- The Current Status and the Perspectives of Nutrition Survey