Clin Exp Otorhinolaryngol.
2013 Mar;6(1):18-22.
Preliminary Findings from Our Experience in Anterior Palatoplasty for the Treatment of Obstructive Sleep Apnea
- Affiliations
-
- 1Head and Neck Surgery Division, San Carlo Hospital, Rome, Italy.
- 2Department of Neurosciences, La Sapienza University of Rome, Rome, Italy.
- 3ENT Clinic, Department of Surgical Sciences, University of Rome "Tor Vergata", Rome, Italy. passali@med.uniroma2.it
Abstract
OBJECTIVES
Obstructive sleep apnea (OSA) is a common disorder affecting at least 2% to 4% of adult population characterized by the collapse of the pharyngeal airway. It is well established that retropalatal region is the most common site of obstruction. Consequently, many surgical techniques have been introduced. The purpose of this study is to present our preliminary results in the anterior palatoplasty (AP) compared with results of uvulopalatal flap (UPF).
METHODS
Thirty-eight consecutive patients with mild-moderate OSA were prospectively enrolled into a randomised surgical protocol. Surgical success was measured primarily by satisfactory reduction in snoring, as reported by snoring assessment questionnaire (SQ) of sleep partners. Secondary outcomes measures included improvement in the Epworth Sleepiness Scale (ESS) scores, changes in the magnitude of pharyngeal collapse, and postoperative pain intensity.
RESULTS
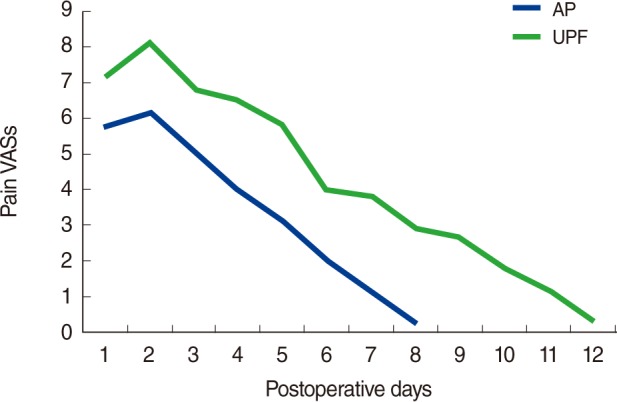
The ESS after AP improved from a preoperative value 8.5+/-3.7 to a postoperative mean of 4.9+/-3.2 (P<0.001) after UPF improved from a preoperative value of 8.1+/-3.5 to 5.2+/-3.2 postoperatively (P<0.001). The results of satisfactory reduction in the volume of snoring and response at polysomnographic data were also similar in both procedures. We reported a statistically significant difference of the collapse noted at Muller manoeuvre that improved from 2.7+/-1.0 on average, to 1.1+/-0.9 (P<0.001) after AP and with a lesser extent, (from 2.8+/-1.1 on average to 1.8+/-1.1; P<0.05), after UPF. The mean duration of pain was 10.8 days for UPF patients and 7.1 days for AP patients. The mean pain score in the first 3 days, was 6.8 in UPF patients and 5.1 in AP patients.
CONCLUSION
The subjective and objective improvements evidenced may suggest how AP is far superior to other techniques aimed at creating a palatal fibrotic scar. In the light of these results we can suggest AP procedure as more practical and comfortable when compared to UPF.
MeSH Terms
Figure
Reference
-
1. Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009; 6. 5(3):263–276. PMID: 19960649.2. Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep. 1997; 9. 20(9):705–706. PMID: 9406321.
Article3. National Commission on Sleep Disorders Research. Wake up America: a national sleep alert. 1995. Washington, DC: National Commission on Sleep Disorders Research.4. Yagi H, Nakata S, Tsuge H, Yasuma F, Noda A, Morinaga M, et al. Morphological examination of upper airway in obstructive sleep apnea. Auris Nasus Larynx. 2009; 8. 36(4):444–449. PMID: 19097716.
Article5. Fujita S, Conway WA, Zorick FJ, Sicklesteel JM, Roehrs TA, Wittig RM, et al. Evaluation of the effectiveness of uvulopalatopharyngoplasty. Laryngoscope. 1985; 1. 95(1):70–74. PMID: 3965833.
Article6. Ellis PD. Laser palatoplasty for snoring due to palatal flutter: a further report. Clin Otolaryngol Allied Sci. 1994; 8. 19(4):350–351. PMID: 7994895.
Article7. Mair EA, Day RH. Cautery-assisted palatal stiffening operation. Otolaryngol Head Neck Surg. 2000; 4. 122(4):547–556. PMID: 10740176.
Article8. Powell N, Riley R, Guilleminault C, Troell R. A reversible uvulopalatal flap for snoring and sleep apnea syndrome. Sleep. 1996; 9. 19(7):593–599. PMID: 8899940.
Article9. Pang KP, Terris DJ. Modified cautery-assisted palatal stiffening operation: new method for treating snoring and mild obstructive sleep apnea. Otolaryngol Head Neck Surg. 2007; 5. 136(5):823–826. PMID: 17478223.
Article10. Sher AE, Schechtman KB, Piccirillo JF. The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep. 1996; 2. 19(2):156–177. PMID: 8855039.
Article11. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008; 2. 5(2):173–178. PMID: 18250209.
Article12. Vicini C, editor. Chirurgia della roncopatia. 2007. Lucca: Eureka.13. Neruntarat C. Uvulopalatal flap for snoring on an outpatient basis. Otolaryngol Head Neck Surg. 2003; 10. 129(4):353–359. PMID: 14574288.
Article14. Pang KP, Tan R, Puraviappan P, Terris DJ. Anterior palatoplasty for the treatment of OSA: three-year results. Otolaryngol Head Neck Surg. 2009; 8. 141(2):253–256. PMID: 19643261.