Korean J Obstet Gynecol.
2011 Jan;54(1):53-56. 10.5468/KJOG.2011.54.1.53.
Sustained fetal sinus bradycardia after maternal cardioversion
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Kyungpook National University School of Medicine, Daegu, Korea. duchess7@naver.com
- KMID: 2274023
- DOI: http://doi.org/10.5468/KJOG.2011.54.1.53
Abstract
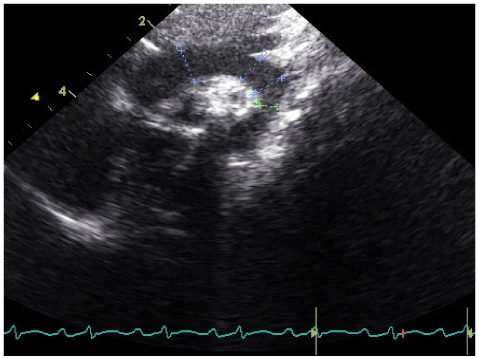
- Direct current cardioversion is reported as a safe procedure during pregnancy. However, the impact of cardioversion on fetal haemodynamics remains unclear. A 28-year-old woman at 10 2/7 weeks of gestation developed shortness of breath while walking. Under the confirmation of atrial flutter by a 12-lead electro-cardiogram, synchronized shock was proceeded at 17 weeks of gestation and the maternal heart rhythm was converted to sinus rhythm. After 3 months, the baseline of fetal heart rate decreased to 110 beats per minute. Fetal bradycardia was aggravated at term, and caesarean section was performed. Following caesarean section, the infant made a full recovery. Although cardioversion during pregnancy is known to be safe, monitoring of fetal heart rate during maternal cardioversion is advisable considering the possibility of severe fetal bradycardia and loss of variability.
MeSH Terms
Figure
Reference
-
1. Chun CS, Yang JI, Lee K, Lee YH, Cho DJ. A clinical study of heart disease in pregnancy. Korean J Obstet Gynecol. 1994. 37:227–232.2. Park HW, Kim SY, Park SH, Lee HY, Rho HS, Oh HM. The perinatal outcomes of pregnant women with cardiac disease. Korean J Obstet Gynecol. 2007. 50:1313–1320.3. Ferrero S, Colombo BM, Ragni N. Maternal arrhythmias during pregnancy. Arch Gynecol Obstet. 2004. 269:244–253.4. Barnes EJ, Eben F, Patterson D. Direct current cardioversion during pregnancy should be performed with facilities available for fetal monitoring and emergency caesarean section. BJOG. 2002. 109:1406–1407.5. Nora JJ, Nora AH. Maternal transmission of congenital heart diseases: new recurrence risk figures and the questions of cytoplasmic inheritance and vulnerability to teratogens. Am J Cardiol. 1987. 59:459–463.6. Wyse RK, Robinson PJ, Deanfield JE, Tunstall Pedoe DS, Macartney FJ. Use of continuous wave Doppler ultrasound velocimetry to assess the severity of coarctation of the aorta by measurement of aortic flow velocities. Br Heart J. 1984. 52:278–283.7. Ino T, Nishimoto K, Kato H, Momma K, Ishizawa A, Kamiya T, et al. Balloon angioplasty for aortic coarctation-report of a questionnaire survey by the Japanese Pediatric Interventional Cardiology Committee. Jpn Circ J. 1997. 61:375–383.8. Wang YC, Chen CH, Su HY, Yu MH. The impact of maternal cardioversion on fetal haemodynamics. Eur J Obstet Gynecol Reprod Biol. 2006. 126:268–269.9. Ueland K, McAnulty JH, Ueland FR, Metcalfe J. Special considerations in the use of cardiovascular drugs. Clin Obstet Gynecol. 1981. 24:809–823.10. Sánchez Díaz CJ, González Carmona VM, Ruesga Zamora E, Monteverde Grether CA. Electric cardioversion in the emergency service: experience in 1000 cases. Arch Inst Cardiol Mex. 1987. 57:387–394.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Electrical Cardioversion of Atrial Fibrillation after Successful Percutaneous Balloon Mitral Valvuloplasty
- A Case of Paroxysmal Atrial Fibrillation and Sinus Bradycardia due to Coronary Artery Spasm
- Maternal-Fetal Interaction Belief and Maternal-Fetal Interaction
- Intrauterine fetal bradycardia after accidental administration of the anesthetic agent in the subdural space during epidural labor analgesia: A case report
- Autonomic imbalance captures maternal and fetal circulatory response to pre-eclampsia