Korean J Obstet Gynecol.
2010 Aug;53(8):746-751. 10.5468/kjog.2010.53.8.746.
Vulva sparganosis misdiagnosed as a Bartholin's gland abscess
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Soonchunhyang University Bucheon Hospital, Bucheon, Korea. hhl22@schbc.ac.kr
- 2Department of Radiology, Soonchunhyang University Bucheon Hospital, Bucheon, Korea.
- 3Department of Pathology, Soonchunhyang University Bucheon Hospital, Bucheon, Korea.
- 4Department of Parasitology, Soonchunhyang University, Seoul, Korea.
- 5Department of Obstetrics and Gynecology, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea.
- KMID: 2273995
- DOI: http://doi.org/10.5468/kjog.2010.53.8.746
Abstract
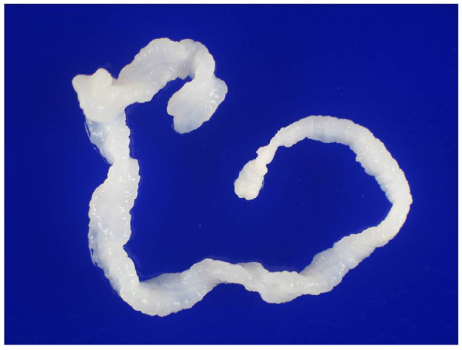
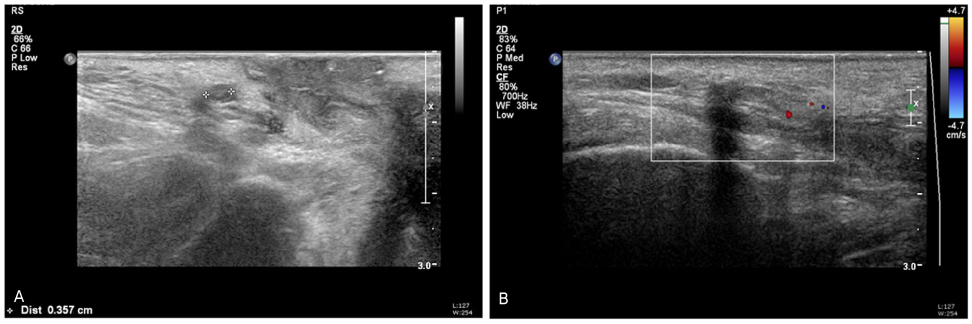
- Sparganosis is a parasitic infection caused by the plerocercoid larvae of diphyllobothroid tapeworms belonging to the genus Spirometra, as first described by Manson in 1882. The infection is transmitted by ingestion of contaminated water, frogs, and snakes, and contact between a second intermediate host and an open wound or mucus membranes. Humans are accidental hosts in the life cycle, but dogs, cats, and other mammals are definitive hosts. Once a human becomes infected, the plerocercoid larvae migrate to a subcutaneous location, where they typically develop into a painful nodule. We misdiagnosed vulva sparganosis as a Bartholin's gland abscess. The patient was a green consumer, so she may have been infected by consuming health foods. Sparganosis should be considered as a cause of soft tissue masses especially among patients who have ingested health foods.
Keyword
MeSH Terms
Figure
Reference
-
1. Cook GC, Zumla AI. Manson's tropical diseases. 2008. 22nd ed. London: Saunders.2. Yang JW, Lee JH, Kang MS. A case of oular sparganosis in Korea. Korean J Ophthalmol. 2007. 21:48–50.3. Phunmanee A, Boonsawat W, Indharapoka B, Tuntisirin C, Kularbkeaw J. Pulmonary sparganosis: a case report with five years follow-up. J Med Assoc Thai. 2001. 84:130–135.4. Shin HB, Lee YW, Lee YK, Koh ES. A case of sparganosis in the soft tissue mass. J Soonchunhyang Med Coll. 2009. 14:807–810.5. Park CK, Ha YS, Huh CW, Song JU. A case of sparganosis in the intradural space of the thoracolumbar spine. J Korean Neurosurg Soc. 1983. 12:739–743.6. Yun SJ, Park MS, Jeon HK, Kim YJ, Kim WJ, Lee SC. A case of vesical and scrotal sparganosis presenting as a scrotal mass. Korean J Parasitol. 2010. 48:57–59.7. Im WS, Han KH, Lim KJ, Lee IS, Park SW. A case of sparganosis in female genitalia. Korean J Obstet Gynecol. 1983. 26:707–710.8. Ahn SK, Lee BJ, Lee SH, Kim SC. Clinical and histopathologic study of sparganosis. Korean J Dermatol. 1992. 30:168–174.9. Lee ES, Hur M, Park HM, Kim SH, Lee JW. A case of sparganosis infestated in the labium major. Korean J Obstet Gynecol. 1995. 38:915–918.10. Margulis AR, Burhenne HJ, Freeny PC, Stevenson GW, editors. Margulis and Burhenne's alimentary tract radiology. 1994. 5th ed. St. Louis: Mosby.11. Guk SM, Seo M, Park YK, Oh MD, Choe KW, Kim JL, et al. Parasitic infections in HIV-infected patients who visited Seoul National University Hospital during the period 1995-2003. Korean J Parasitol. 2005. 43:1–5.12. Lee SH, Chai JY, Hong ST. Synopsis of medical parasitology. 1996. Seoul: Korea Medical Book Publishing Co.;272–277.13. McKerrow JH, Brindley P, Brown M, Gam AA, Staunton C, Neva FA. Strongyloides stercoralis: identification of a protease that facilitates penetration of skin by the infective larvae. Exp Parasitol. 1990. 70:134–143.14. Han SJ, Jung JI, Song KE. A case of sparganosis infesting in the labia majora. Korean J Obstet Gynecol. 1991. 34:1646–1650.15. Beaver DC, Jung RC, Cupp EW. Clinical parasitology. 1984. 9th ed. Philadelphia: Lea & Febriger.16. Song HO, Ahn MH, Choi HK, Ryu JS, Min DY, Ree HI. Analysis of 205 cases of parasite infection confirmed in clinical specimens. Korean J Clin Microbiol. 2004. 7:66–71.17. Choi WH, Chu JP, Jiang M, Lee YS, Kim BS, Kim DG, et al. Analysis of parasitic diseases diagnosed by tissue biopsy specimens at KyungHee Medical Center (1984-2005) in Seoul, Korea. Korean J Parasitol. 2010. 48:85–88.18. Wang KC, Huh S, Hong ST, Chai JY, Choi KS, Lee SH. The fate of spargana inoculated into the cat brain and sequential changes of anti-sparganum IgG antibody levels in the cerebrospinal fluid. Korean J Parasitol. 1990. 28:1–10.19. Kim J, Park JH, Ryu YH, Lee KY. Tc-99m ECD SPECT and FDG PET in partial status epilepticus resulting from cerebral sparganosis. Clin Nucl Med. 2006. 31:307–309.20. Chai JY, Yu JR, Lee SH, Kim SI, Cho SY. Ineffectiveness of praziquantel treatment for human sparganosis (a case report). Seoul J Med. 1988. 29:397–399.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Complication of Crohn's disease on the vulva treated as a Bartholin's gland abscess: A case report
- Radiation Treatment for Primary Adenocarcinoma of Bartholin's Gland: A Case Report and Review of Literature
- A Case of Hemorrhagic Huge Bartholin Abscess
- Two Cases of Adenoid Cystic Carcinoma of the Bartholin's Gland
- Bilateral Bartholin's Gland Hyperplasia Associated with Bartholin's Gland Cyst: A Brief Case Report