Korean J Obstet Gynecol.
2010 Mar;53(3):282-286. 10.5468/kjog.2010.53.3.282.
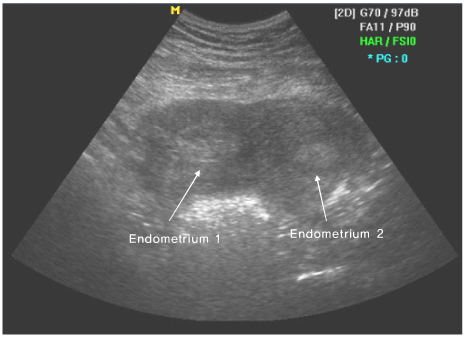
A case of placental abruption diagnosed at 31 weeks by ultrasonography in bicornuate uterus
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Soonchunhyang University College of Medicine, Soonchunhyang University Chunan Hospital, Chunan, Korea. drsook@schca.ac.kr
- KMID: 2273854
- DOI: http://doi.org/10.5468/kjog.2010.53.3.282
Abstract
- Placental abruption is defined as the early separation a normal placenta from the wall of the uterus before delivery of the fetus. The incidence of it is known 1% of all pregnancies and perinatal mortality rates from abruption range from 20% to 40% in recent studies. The most common symptom is vaginal bleeding. The causes are associated with preeclampsia, other hypertensive disorders, and premature rupture of membranes. It is diagnosed by clinical symptom, sign, and ultrasonography. Recently we have experienced a case of placental abruption diagnosed at 31 weeks by ultrasonography in bicornuate uterus with a brief review of the literature.
MeSH Terms
Figure
Reference
-
2. Cunningham FG, Williams JW. Williams Obstetrics. 2009. 23rd ed. New York: McGraw-Hill Medical;787–789.3. Longo LD. Classic pages in Obstetrics and Gynecology. An essay on the uterine hemorrhage, which precedes the delivery of the full grown fetus: illustrated with cases. Am J Obstet Gynecol. 1977. 129:825–826.4. Combs CA, Nyberg DA, Mack LA, Smith JR, Bneditti TJ. Expectant management after sonographic diagnosis of placental abruption. Am J Perinatol. 1992. 9:170–174.
Article6. Ananth CV, Wilcox AJ. Placental abruption and perinatal mortality in the United States. Am J epidemiol. 2001. 153:332–337.
Article8. Ananth CV, Cavitz DA, Williams MA. Placental abruption and its association with hypertension and prolonged rupture of membranes: a methodologic review and meta-analysis. Obstet Gynecol. 1996. 88:309–318.9. Kåregård M, Gennser G. Incidence and recurrence rate of abruptio placentae in Sweden. Obstet Gynecol. 1986. 67:523–528.10. Hurd WW, Miodovnik M, Hertzgerg V, Lavin JP. Selective management of abruptio placentae: A prospective study. Obstet Gynecol. 1983. 61:467–473.12. Nyberg DA, Cyr DR, Mack LA, Wilson DA, Schuman WP. Sonographic spectrum of placental abruption. AJR Am J Roentgenol. 1987. 148:161–164.
Article13. Sholl JS. Abruptio placentae: Clinical management in nonacute cases. Am J Obstet Gynecol. 1987. 156:40–51.
Article14. Glantz C, Purnell L. Clinical utility of sonography in the diagnosis and treatment of placental abruption. J Ultrasound Med. 2002. 21:837–839.
Article16. Harris Ba Jr. Peripheral placental separation: A review. Obstet Gynecol Survey. 1988. 43:577–581.
Article17. Bond AL, Fdersheim TG, Curry L, Druzin MI, Hutson JM. Expectant management of abruptio placentae before 35 weeks gestation. Am J Perinatol. 1989. 6:121–123.
Article18. Page EW, King EB, Merill JA. Abruptio placentae: Dangers of delay in delivery. Obstet Gynecol. 1954. 3:385–393.19. Newton ER, Kennedy JL Jr, Louis F, Cetrulo CL, Sbarra A, Feingold M. Obstetric diagnosis and perinatal mortality. Am J Perinatol. 1987. 4:300–304.
Article20. Gonen R, Hannah ME, Milligan JE. Does prolonged preterm rupture of the membranes predispose to abruptio placentae? Obstet Gynecol. 1989. 74(3 Pt 1):347–350.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Chronic Placental Abruption-Oligohydramnios Sequence at 19 Weeks' Gestation
- Treatment of placental abruption following blunt abdominal trauma: a case report
- Clinical study on obstetric variables affecting perinatal mortality in placental abruption
- Congenital Uterine Anomaly and Pelvic Organ Prolapse: A Rare Case of Pelvic Organ Prolapse in a Complete Bicornuate Uterus with Successful Pregnancy Outcomes Undiagnosed until the Time of Sacrocolpopexy
- A Case Of Dis (Disserninated Intravascular Coagulation) With Placental Abruption In 16 Weeks Of Gestational Age