Korean J Orthod.
2014 Jul;44(4):203-216. 10.4041/kjod.2014.44.4.203.
Treatment and retention of relapsed anterior open-bite with low tongue posture and tongue-tie: A 10-year follow-up
- Affiliations
-
- 1Department of Orthodontics, School of Dentistry, Kyunghee University, Seoul, Korea. bravortho@catholic.ac.kr
- 2Department of Orthodontics, School of Medicine, Ajou University, Suwon, Korea.
- 3Department of Orthodontics, School of Dentistry, West Virginia University, Morgantown, WV, USA.
- KMID: 2273277
- DOI: http://doi.org/10.4041/kjod.2014.44.4.203
Abstract
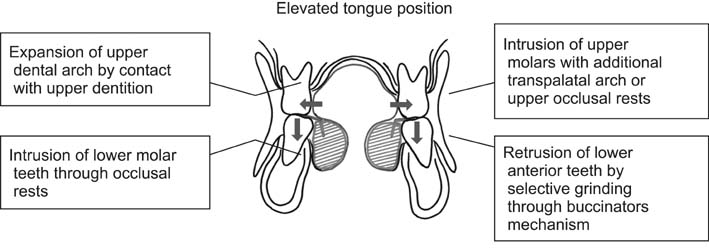
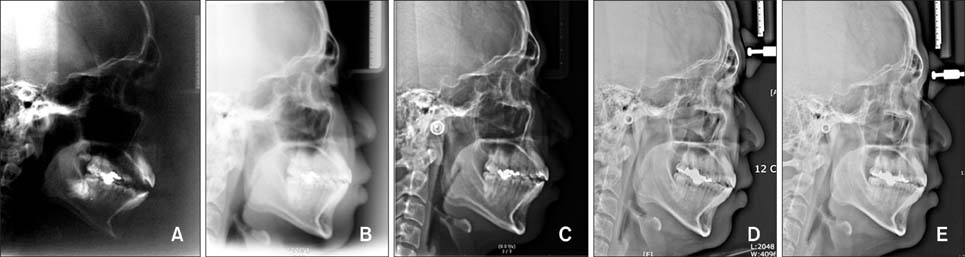
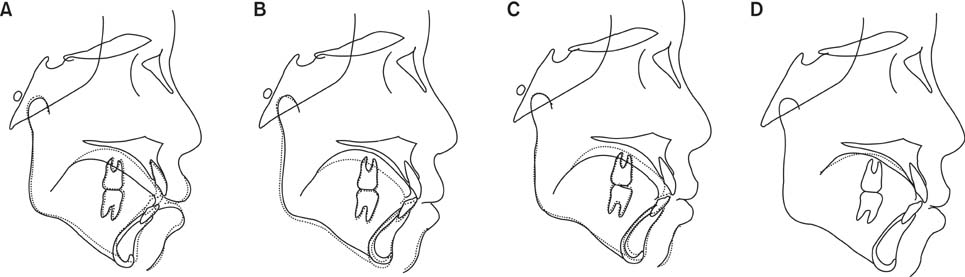
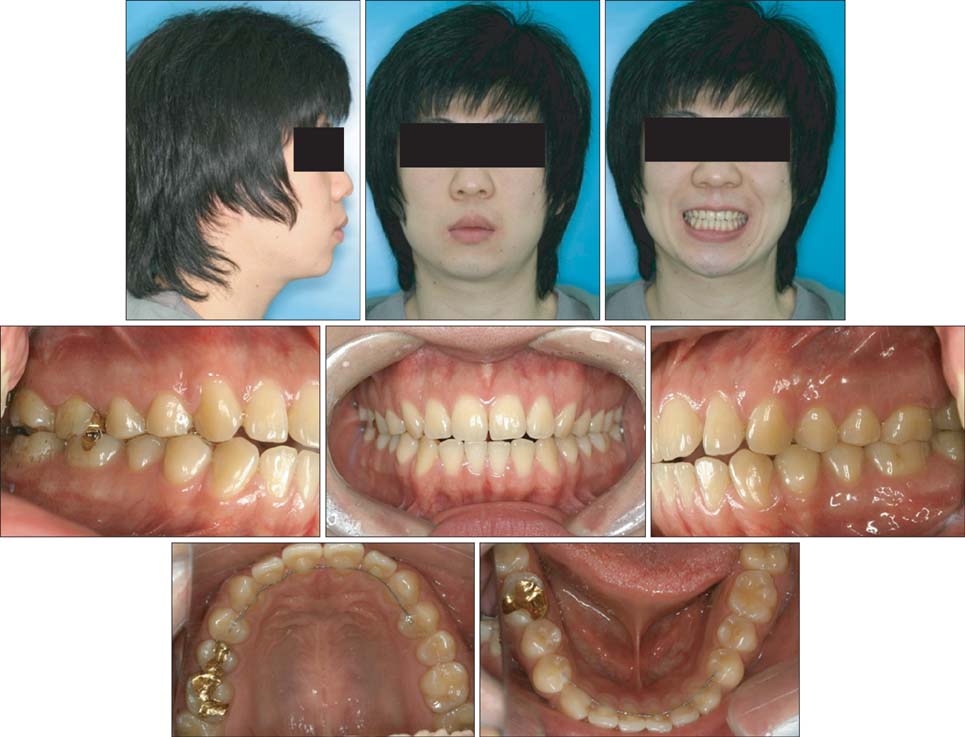
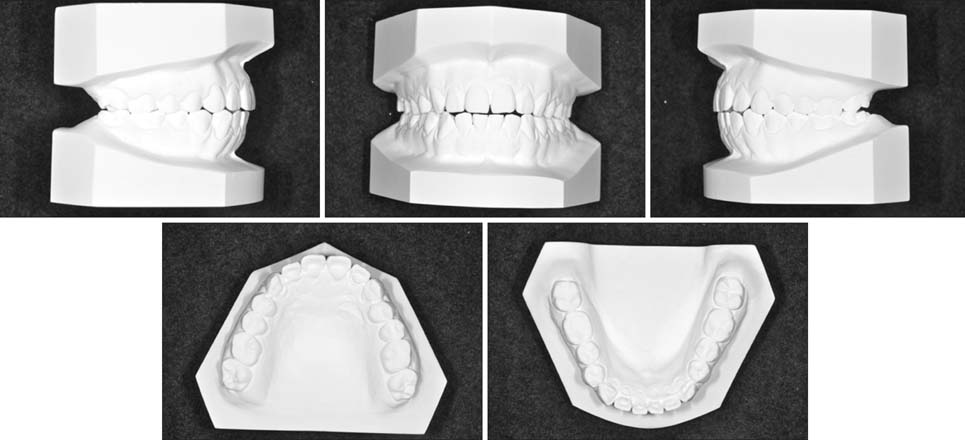
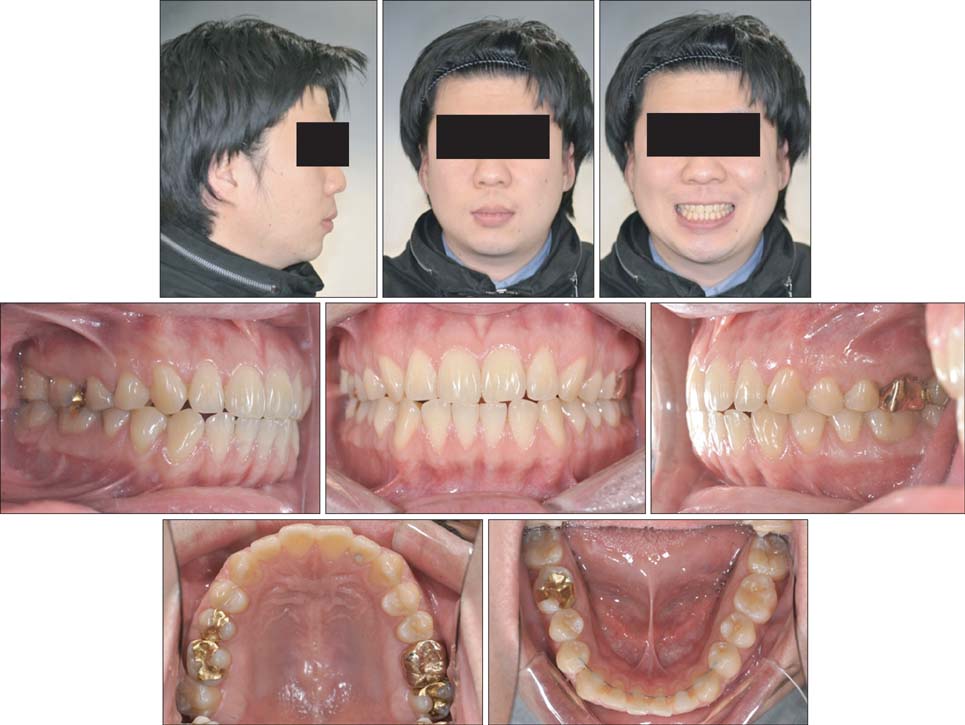
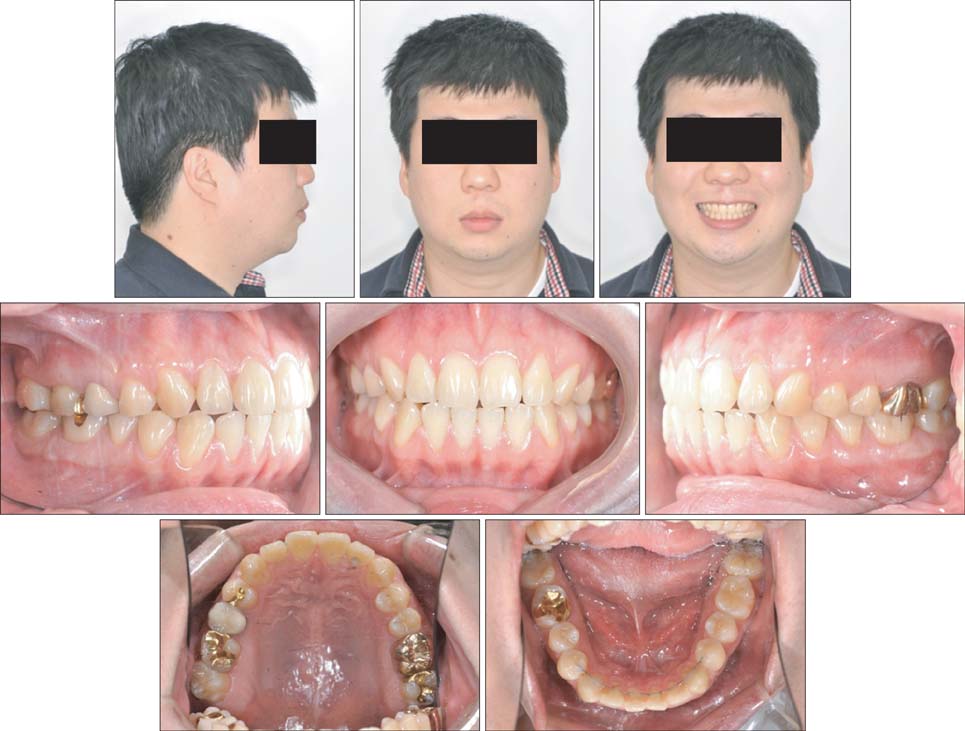
- The purpose of the current report is to present 6-year long-term stability and 10-year follow-up data for an adult patient who was treated with a tongue elevator for relapsed anterior open-bite. The 19-year-old male patient presented with the chief complaint of difficulty in chewing his food. Collectively, clinical and radiographic examinations revealed an anterior open-bite, low tongue posture, and tongue-tie. The patient opted for orthodontic treatment alone, without any surgical procedure. A lingual frenectomy was recommended to avoid the risk of relapse, but the patient declined because he was not experiencing tongue discomfort. Initial treatment of the anterior open-bite with molar intrusion and tongue exercises was successful, but relapse occurred during the retention period. A tongue elevator was used for retreatment, because the approach was minimally invasive and suited the patient's requirements regarding discomfort, cost, and time. The appliance changed the tongue posture and generated an altered tongue force, which ultimately resulted in intrusive dentoalveolar effects, and a subsequent counterclockwise rotation of the mandible. The results showed long-term stability and were maintained for six years through continual use of the tongue elevator. The results of this case indicated that a tongue elevator could be used not only as an alternative treatment for open-bite, but also as an active retainer.
Keyword
MeSH Terms
Figure
Reference
-
1. Proffit WR. Equilibrium theory revisited: factors influencing position of the teeth. Angle Orthod. 1978; 48:175–186.2. Proffit WR. On the aetiology of malocclusion. The Northcroft lecture, 1985 presented to the British Society for the Study of Orthodontics, Oxford, April 18, 1985. Br J Orthod. 1986; 13:1–11.3. Horton CE, Crawford HH, Adamson JE, Ashbell TS. Tongue-tie. Cleft Palate J. 1969; 6:8–23.4. Proffit WR, Mason RM. Myofunctional therapy for tongue-thrusting: background and recommendations. J Am Dent Assoc. 1975; 90:403–411.
Article5. Yamaguchi H, Sueishi K. Malocclusion associated with abnormal posture. Bull Tokyo Dent Coll. 2003; 44:43–54.
Article6. Tsuiki S, Handa S, Ohyama K. A simple method for evaluation of tongue position. J Oral Rehabil. 2007; 34:304–310.
Article7. Huang GJ, Justus R, Kennedy DB, Kokich VG. Stability of anterior openbite treated with crib therapy. Angle Orthod. 1990; 60:17–24. discussion 25-6.8. de Cuebas JO. Nonsurgical treatment of a skeletal vertical discrepancy with a significant open bite. Am J Orthod Dentofacial Orthop. 1997; 112:124–131.
Article9. Taslan S, Biren S, Ceylanoglu C. Tongue pressure changes before, during and after crib appliance therapy. Angle Orthod. 2010; 80:533–539.
Article10. Hotokezaka H, Matsuo T, Nakagawa M, Mizuno A, Kobayashi K. Severe dental open bite malocclusion with tongue reduction after orthodontic treatment. Angle Orthod. 2001; 71:228–236.11. Liu ZJ, Shcherbatyy V, Gu G, Perkins JA. Effects of tongue volume reduction on craniofacial growth: A longitudinal study on orofacial skeletons and dental arches. Arch Oral Biol. 2008; 53:991–1001.
Article12. Chatzistavrou E, Kolokitha OE, Topouzelis N. A severe open bite case treated with orthodontics and tongue reduction surgery: 13-year followup. A case report. Aust Orthod J. 2012; 28:94–103.13. Takahashi O, Iwasawa T, Takahashi M. Integrating orthodontics and oral myofunctional therapy for patients with oral myofunctional disorders. Int J Orofacial Myology. 1995; 21:66–72.
Article14. Smithpeter J, Covell D Jr. Relapse of anterior open bites treated with orthodontic appliances with and without orofacial myofunctional therapy. Am J Orthod Dentofacial Orthop. 2010; 137:605–614.
Article15. Messner AH, Lalakea ML. Ankyloglossia: controversies in management. Int J Pediatr Otorhinolaryngol. 2000; 54:123–131.
Article16. García Pola MJ, González García M, García Martín JM, Gallas M, Seoane Lestón J. A study of pathology associated with short lingual frenum. ASDC J Dent Child. 2002; 69:59–62. 1217. Ruffoli R, Giambelluca MA, Scavuzzo MC, Bonfigli D, Cristofani R, Gabriele M, et al. Ankyloglossia: a morphofunctional investigation in children. Oral Dis. 2005; 11:170–174.
Article18. Suter VG, Bornstein MM. Ankyloglossia: facts and myths in diagnosis and treatment. J Periodontol. 2009; 80:1204–1219.
Article19. Chung KR. Clinical dental orthodontics. Seoul, Korea: Myung Moon Pub Co;1998.20. Kim YS, Kown SY, Park YG, Chung KR. Clinical application of the tongue elevator. J Clin Orthod. 2002; 36:104–106.21. Ozbek MM, Memikoglu UT, Altug-Atac AT, Lowe AA. Stability of maxillary expansion and tongue posture. Angle Orthod. 2009; 79:214–220.
Article22. Lopez-Gavito G, Wallen TR, Little RM, Joondeph DR. Anterior open-bite malocclusion: a longitudinal 10-year postretention evaluation of orthodontically treated patients. Am J Orthod. 1985; 87:175–186.
Article23. Lentini-Oliveira D, Carvalho FR, Qingsong Y, Junjie L, Saconato H, Machado MA, et al. Orthodontic and orthopaedic treatment for anterior open bite in children. Cochrane Database Syst Rev. 2007; (2):CD005515.
Article24. Greenlee GM, Huang GJ, Chen SS, Chen J, Koepsell T, Hujoel P. Stability of treatment for anterior open-bite malocclusion: a meta-analysis. Am J Orthod Dentofacial Orthop. 2011; 139:154–169.
Article25. Tanaka E, Yamano E, Inubushi T, Kuroda S. Management of acquired open bite associated with temporomandibular joint osteoarthritis using miniscrew anchorage. Korean J Orthod. 2012; 42:144–154.
Article26. Sugawara J, Baik UB, Umemori M, Takahashi I, Nagasaka H, Kawamura H, et al. Treatment and posttreatment dentoalveolar changes following intrusion of mandibular molars with application of a skeletal anchorage system (SAS) for open bite correction. Int J Adult Orthodon Orthognath Surg. 2002; 17:243–253.27. Baek MS, Choi YJ, Yu HS, Lee KJ, Kwak J, Park YC. Long-term stability of anterior open-bite treatment by intrusion of maxillary posterior teeth. Am J Orthod Dentofacial Orthop. 2010; 138:396.e1–396.e9. discussion 396-8.
Article28. Volk J, Kadivec M, Mušič MM, Ovsenik M. Three-dimensional ultrasound diagnostics of tongue posture in children with unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 2010; 138:608–612.
Article29. Iwasaki T, Saitoh I, Takemoto Y, Inada E, Kakuno E, Kanomi R, et al. Tongue posture improvement and pharyngeal airway enlargement as secondary effects of rapid maxillary expansion: a cone-beam computed tomography study. Am J Orthod Dentofacial Orthop. 2013; 143:235–245.
Article30. Hohoff A, Ehmer U. Effects of the Castillo-Morales stimulating plate on speech development of children with Down's syndrome. A retrospective study. J Orofac Orthop. 1997; 58:330–339.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An electromyograghic study of muscular activities of tongue and lip muscles in anterior open-bite
- Multidisciplinary correction of anterior open bite relapse and upper airway obstruction
- Central tongue reduction for macroglossia
- A comparative study on the genioglossus muscle and orbicularis oris muscle activity in the anterior open bite and normal occlusion
- A case report of orthodontic treatment of anterior open bite