Ann Rehabil Med.
2015 Feb;39(1):108-115. 10.5535/arm.2015.39.1.108.
Pain-Related Evoked Potential in Healthy Adults
- Affiliations
-
- 1Department of Rehabilitation Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea. invisibleangel@hanmail.net
- KMID: 2273026
- DOI: http://doi.org/10.5535/arm.2015.39.1.108
Abstract
OBJECTIVE
To investigate the normal data of pain-related evoked potentials (PREP) elicited with a concentric surface electrode among normal, healthy adults and the relationship between PREP and pain intensity.
METHODS
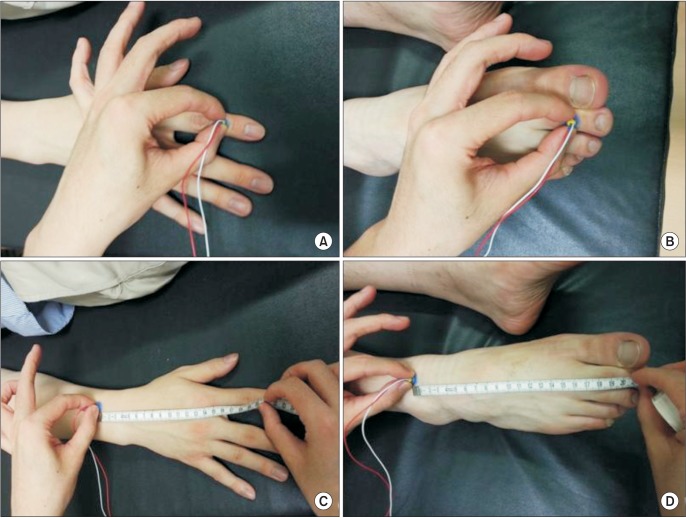
Sixty healthy volunteers (22 men and 38 women; aged 36.4+/-10.7 years; height, 165.4+/-7.8 cm) were enrolled. Routine nerve conduction study (NCS) was done to measure PREP following electrical stimulation of hands (C7 dermatome) and feet (L5 dermatome). Negative peak (N), positive peak (P) latencies, peak to peak (NP) amplitudes, conduction velocity (CV), and verbal rating scale (VRS) score were obtained. Linear regression analysis tested for significant relevance between variables of PREP and VRS score.
RESULTS
Normal NCS results were obtained in all subjects. N latency of hand PREP was 163.8 +/-40.0 ms (right) and 161.0+/-39.9 ms (left). N latency of foot PREP was 178.0+/-43.9 ms (right), 180.4+/-43.4 ms (left). NP amplitude of hands was 20.6+/-10.6 microV (right) and 21.9+/-11.6 microV (left). NP amplitude of feet was 18.8+/-8.3 microV (right) and 19.0+/-8.4 microV (left). The calculated CV was 13.2+/-4.7 m/s and VRS score was 3.8+/-1.0. A highly significant positive correlation was evident between VRS score and NP amplitude (y=0.1069x+1.781, r=0.877, n=60, p<0.0001).
CONCLUSION
PREP among normal, healthy adults revealed a statistically significant correlation between PREP amplitude and VRS score.
MeSH Terms
Figure
Cited by 1 articles
-
Measurement of Knee Extensor Torque During Repetitive Peripheral Magnetic Stimulation: Comparison of the Forces Induced by Different Stimulators
Masanori Kamiue, Akio Tsubahara, Tomotaka Ito, Yasuhiro Koike
Ann Rehabil Med. 2024;48(3):203-210. doi: 10.5535/arm.230025.
Reference
-
1. Katsarava Z, Ayzenberg I, Sack F, Limmroth V, Diener HC, Kaube H. A novel method of eliciting pain-related potentials by transcutaneous electrical stimulation. Headache. 2006; 46:1511–1517. PMID: 17115984.
Article2. Valeriani M, Le Pera D, Niddam D, Chen AC, Arendt-Nielsen L. Dipolar modelling of the scalp evoked potentials to painful contact heat stimulation of the human skin. Neurosci Lett. 2002; 318:44–48. PMID: 11786221.
Article3. Katsarava Z, Yaldizli O, Voulkoudis C, Diener HC, Kaube H, Maschke M. Pain related potentials by electrical stimulation of skin for detection of small-fiber neuropathy in HIV. J Neurol. 2006; 253:1581–1584. PMID: 17063317.
Article4. Beydoun A, Morrow TJ, Shen JF, Casey KL. Variability of laser-evoked potentials: attention, arousal and lateralized differences. Electroencephalogr Clin Neurophysiol. 1993; 88:173–181. PMID: 7684966.
Article5. Bromm B, Jahnke MT, Treede RD. Responses of human cutaneous afferents to CO2 laser stimuli causing pain. Exp Brain Res. 1984; 55:158–166. PMID: 6086371.
Article6. Kakigi R, Shibasaki H, Ikeda A. Pain-related somatosensory evoked potentials following CO2 laser stimulation in man. Electroencephalogr Clin Neurophysiol. 1989; 74:139–146. PMID: 2465889.7. Kaube H, Katsarava Z, Kaufer T, Diener H, Ellrich J. A new method to increase nociception specificity of the human blink reflex. Clin Neurophysiol. 2000; 111:413–416. PMID: 10699400.
Article8. Katsarava Z, Ellrich J, Diener HC, Kaube H. Optimized stimulation and recording parameters of human 'nociception specific' blink reflex recordings. Clin Neurophysiol. 2002; 113:1932–1936. PMID: 12464330.
Article9. Ayzenberg I, Obermann M, Nyhuis P, Gastpar M, Limmroth V, Diener HC, et al. Central sensitization of the trigeminal and somatic nociceptive systems in medication overuse headache mainly involves cerebral supraspinal structures. Cephalalgia. 2006; 26:1106–1114. PMID: 16919061.
Article10. Katsarava Z, Lehnerdt G, Duda B, Ellrich J, Diener HC, Kaube H. Sensitization of trigeminal nociception specific for migraine but not pain of sinusitis. Neurology. 2002; 59:1450–1453. PMID: 12427905.
Article11. Kaube H, Katsarava Z, Przywara S, Drepper J, Ellrich J, Diener HC. Acute migraine headache: possible sensitization of neurons in the spinal trigeminal nucleus? Neurology. 2002; 58:1234–1238. PMID: 11971092.
Article12. Mueller D, Obermann M, Koeppen S, Kavuk I, Yoon MS, Sack F, et al. Electrically evoked nociceptive potentials for early detection of diabetic small-fiber neuropathy. Eur J Neurol. 2010; 17(6):834–841. PMID: 20192984.
Article13. Kanda M, Matsuhashi M, Sawamoto N, Oga T, Mima T, Nagamine T, et al. Cortical potentials related to assessment of pain intensity with visual analogue scale (VAS). Clin Neurophysiol. 2002; 113:1013–1024. PMID: 12088694.
Article14. Tran TD, Lam K, Hoshiyama M, Kakigi R. A new method for measuring the conduction velocities of Abeta-, Adelta- and C-fibers following electric and CO(2) laser stimulation in humans. Neurosci Lett. 2001; 301:187–190. PMID: 11257429.15. Inui K, Tran TD, Hoshiyama M, Kakigi R. Preferential stimulation of Adelta fibers by intra-epidermal needle electrode in humans. Pain. 2002; 96:247–252. PMID: 11972996.17. Polydefkis M, Yiannoutsos CT, Cohen BA, Hollander H, Schifitto G, Clifford DB, et al. Reduced intraepidermal nerve fiber density in HIV-associated sensory neuropathy. Neurology. 2002; 58:115–119. PMID: 11781415.
Article18. Tagliati M, Grinnell J, Godbold J, Simpson DM. Peripheral nerve function in HIV infection: clinical, electrophysiologic, and laboratory findings. Arch Neurol. 1999; 56:84–89. PMID: 9923765.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Tendon Reflex Responses between Two Heads of Gastrocnemius in Spastic Hemiplegia and Healthy Subjects
- The Effect of Lorazepam on the Silent Period of the Motor Evoked Potential
- Evoked Potentials in Wilson Disease
- Visual Evoked Potential Study in Amblyopia and Normal Groups
- Effect of Different Sites of Recording Electrodes on Auditory Evoked Potentials in Healthy Adults