Ann Rehabil Med.
2011 Jun;35(3):395-404. 10.5535/arm.2011.35.3.395.
Usefulness of Posterolateral Transforaminal Approach in Lumbar Radicular Pain
- Affiliations
-
- 1Department of Rehabilitation Medicine, Soonchunhyang University College of Medicine, Seoul 140-887, Korea.
- 2Department of Rehabilitation Medicine, Hallym University College of Medicine, Seoul 134-814, Korea.
- 3Department of Rehabilitation Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul 139-707, Korea. swc328@naver.com
- KMID: 2266860
- DOI: http://doi.org/10.5535/arm.2011.35.3.395
Abstract
OBJECTIVE
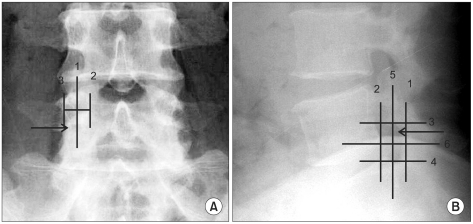
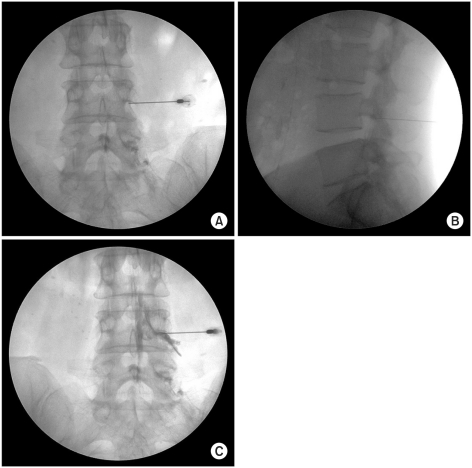
To compare the short-term effects and advantages of transforaminal epidural steroid injection (TFESI) performed using the conventional (CL) and posterolateral (PL) approaches. METHOD: Fifty patients with lumbar radicular pain from lumbar spinal stenosis and herniated lumbar disc were enrolled. Subjects were randomly assigned to one of two groups (CL or PL group). All procedures were performed using a C-arm (KMC 950, KOMED, Kwangju, Kyunggi, Korea). We compared the frequency of complications during the procedure and the effects of the pain block between the two groups at 2, 4, and 12 weeks after the procedure.
RESULTS
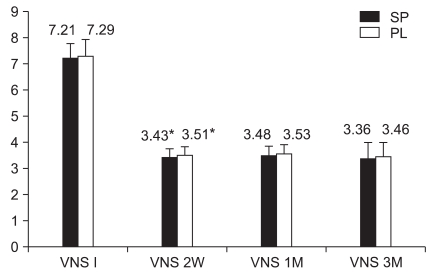
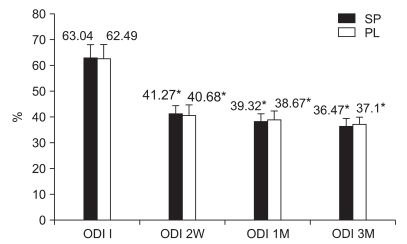
There were no significant differences in the demographic data, initial VNS (Visual numeric scale), or ODI (Oswestry disability index) between the CL group (n=26) and the PL group (n=24). There was no statistically significant difference in the outcome measures (VNS and ODI) between the groups at 2, 4, or 12 weeks. Symptoms of nerve root irritation occurred in 1 case of the CL group and in 7 cases of the PL group (p<0.05). Pricking of spinal nerve during the procedure and transient weakness after the procedure occurred in 6 cases and 3 cases, respectively in the CL group, but did not occur in the PL group.
CONCLUSION
Our findings suggest that the posterolateral approach represents an alternative TFESI method in cases with difficult needle tip positioning in the anterior epidural space, and could lower the risk of target nerve root irritation and nerve penetration.
Keyword
Figure
Reference
-
1. Slipman CW, Chow DW. Therapeutic spinal corticosteroid injections for the management of radiculopathies. Phys Med Rehabil Clin N Am. 2002; 13:697–711. PMID: 12380554.
Article2. Manchikanti L, Staats PS, Singh V, Schultz DM, Vilims BD, Jasper JF, Kloth DS, Trescot AM, Hansen HC, Falasca TD, et al. Evidence-based practice guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2003; 6:3–81. PMID: 16878163.3. Abdi S, Datta S, Trescot AM, Schultz DM, Adlaka R, Atluri SL, Smith HS, Manchi kanti L. Epidural steroids in the management of chronic spinal pain: a systematic review. Pain Physician. 2007; 10:185–212. PMID: 17256030.4. Manchikanti L. Transforaminal lumbar epidural steroid injections. Pain Physician. 2000; 3:374–398. PMID: 16906179.
Article5. Bogduk N. Clinical anatomy of the lumbar spine and sacrum. 2005. 4th ed. New York: churchill Living stone;p. 123–124.6. Eriksen W. The prevalence of musculoskeletal pain in Norwegian nurses' aides. Int Arch Occup Environ Health. 2003; 76:625–630. PMID: 14520578.
Article7. Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Sanelli JT, Freeman ED, Slaten WK, Rao S. Fluoroscopically guided lumbar transforaminal epidural steroid injections in degenerative lumbar stenosis: an outcome study. Am J Phys Med Rehabil. 2002; 81:898–905. PMID: 12447088.8. Lee IS, Kim SH, Lee JW, Hong SH, Choi JY, Kang HS, Song JW, Kwon AK. Comparison of the temporary dia gnostic relief of transforaminal epidural steroid injection approaches: conventional versus posterolateral technique. AJNR Am J Neuroradiol. 2007; 28:204–208. PMID: 17296980.9. Houten JK, Errico TJ. Paraplegia after lumbosacral nerve root block: report of three cases. Spine J. 2002; 2:70–75. PMID: 14588291.10. Somayaji HS, Saifuddin A, Casey AT, Briggs TW. Spinal cord infarction following therapeutic computed tomography-guided left L2 nerve root injection. Spine. 2005; 30:E106–E108. PMID: 15706327.
Article11. Stretanski MF, Chopko B. Unintentional vascular uptake in fluoroscopically guided, contrast-confirmed spinal injections: a 1-yr clinical experience and discussion of findings. Am J Phys Med Rehabil. 2005; 84:30–35. PMID: 15632486.12. Crall TS, Gilula LA, Kim YJ, Cho Y, Pilgram T, Riew KD. The diagnostic effect of various needle tip positions in selective lumbar nerve blocks: an analysis of 1202 injections. Spine. 2006; 31:920–922. PMID: 16622382.
Article13. Nygaard OP, Mellgren SI, Osterud B. The inflammatory properties of contained and noncontained lumbar disc herniation. Spine. 1997; 22:2484–2488. PMID: 9383853.
Article14. Franson RC, Saal JS, Saal JA. Human disc phospholipase A2 is inflammatory. Spine (Phila Pa 1976). 1992; 17(6 Suppl):S129–S132. PMID: 1631712.
Article15. Olmarker K, Blomquist J, Stromberg J, Nannmark U, Thomsen P, Rydevik B. Inflammatogenic properties of nucleus pulposus. Spine. 1995; 20:665–669. PMID: 7604342.
Article16. Rydevik B, Brown MD, Lundborg G. Pathoanatomy and pathophysiology of nerve root compression. Spine. 1984; 9:7–15. PMID: 6372124.
Article17. Kantrowitz F, Robinson DR, McGuire MB, Levine L. Corticosteroids inhibit prostaglandin production by rheumatoid synovia. Nature. 1975; 258:737–739. PMID: 1207758.
Article18. Fukusaki M, Kobayashi I, Hara T, Sumikawa K. Symptoms of spinal stenosis do not improve after epidural steroid injection. Clin J Pain. 1998; 14:148–151. PMID: 9647457.
Article19. Johansson A, Hao J, Sjolund B. Local corticosteroid application blocks transmission in normal nociceptor C-fibres. Acta Anaesthesiol Scand. 1990; 34:335–338. PMID: 2167604.20. Aprill CN, Melfi RS. Paraplegia after lumbosacral nerve block: report of three cases. Spine J. 2004; 4:368–369. PMID: 15125864.21. Bogduk N, Wilson AS, Tynan W. The human lumbar dorsal rami. J Anat. 1982; 134:383–397. PMID: 7076562.22. Goodman BS, Bayazitoglu M, Mallempati S, Noble BR, Geffen JF. Dural puncture and subdural injection: a complication of lumbar transforaminal epidural injections. Pain Physician. 2007; 10:697–705. PMID: 17876368.23. Hamanishi C, Tanaka S. Dorsal root ganglia in the lumbosacral region observed from the axial views of MRI. Spine. 1993; 18:1753–1756. PMID: 8235857.
Article24. Lehmann LJ, Pallares VS. Subdural injection of a local anesthetic with steroids: complication of epidural anesthesia. South Med J. 1995; 88:467–469. PMID: 7716603.25. Sullivan WJ, Willick SE, Chira-Adisai W, Zuhosky J, Tyburski M, Dreyfuss P, Prather H, Press JM. Incidence of intravascular uptake in lumbar spinal injection procedures. Spine. 2000; 25:481–486. PMID: 10707395.
Article26. Furman MB, O'Brien EM, Zgleszewski TM. Incidence of intravascular penetration in transforaminal lumbosacral epidural steroid injections. Spine. 2000; 25:2628–2632. PMID: 11034648.
Article27. Furman MB, Giovanniello MT, O'Brien EM. Incidence of intravascular penetration in transforaminal cervical epidural steroid injections. Spine. 2003; 28:21–25. PMID: 12544950.
Article28. Smuck M, Fuller BJ, Yoder B, Huerta J. Incidence of simultaneous epidural and vascular injection during lumbosacral transforaminal epidural injections. Spine J. 2007; 7:79–82. PMID: 17197337.
Article29. Derby R, Lee SH, Kim BJ, Chen Y, Seo KS. Complications following cervical epidural steroid injections by expert interventionalists in 2003. Pain Physician. 2004; 7:445–449. PMID: 16858486.30. Alleyne CH Jr, Cawley CM, Shengelaia GG, Barrow DL. Microsurgical anatomy of the artery of Adamkiewicz and its segmental artery. J Neurosurg. 1998; 89:791–795. PMID: 9817417.
Article31. Burn JM, Langdon L. Lumbar epidural injection for the treatment of chronic sciatica. Rheum Phys Med. 1970; 10:368–374.
Article32. Snoek W, Weber H, Jorgensen B. Double blind evaluation of extradural methyl prednisolone for herniated lumbar discs. Acta Orthop Scand. 1977; 48:635–641. PMID: 343479.
Article33. Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Freeman TL, Slaten WK. Complications of fluoroscopically guided transforaminal lumbar epidural injections. Arch Phys Med Rehabil. 2000; 81:1045–1050. PMID: 10943753.
Article34. Pfirrmann CW, Oberholzer PA, Zanetti M, Boos N, Trudell DJ, Resnick D, Hodler J. Selective nerve root blocks for the treatment of sciatica: evaluation of injection site and effectiveness: a study with patients and cadavers. Radiology. 2001; 221:704–711. PMID: 11719666.35. Bogduk N. Epidural steroids. Spine. 1995; 20:845–848. PMID: 7701401.36. Huson A, Luyendijk W, Tielbeek A, Van Zundert A. CT-epidurography and the anatomy of the human lumbar epidural space. Anesthesiology. 1988; 69:797–798. PMID: 3189934.
Article37. Thomas E, Cyteval C, Abiad L, Picot MC, Taourel P, Blotman F. Efficacy of transforaminal versus interspinous corticosteroid injection in discal radiculalgia-a prospective, randomized, double-blind study. Clin Rheumatol. 2003; 22:299–304. PMID: 14579160.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Translaminar Approach and Transforaminal Approach in Lumbar Epidural Steroid Injection
- Effect of Transforaminal Epidural Injection in Patients with Lumbar Radicular Pain
- High Lumbar Disc Herniation Treated with A Modified Posterolateral Approach: Case Report
- Oblique interlaminar lumbar epidural steroid injection for management of low back pain with lumbosacral radicular pain: A case report
- Comparison of Morphine and Tramadol in Transforaminal Epidural Injections for Lumbar Radicular Pain