Ann Rehabil Med.
2012 Aug;36(4):521-529. 10.5535/arm.2012.36.4.521.
Feasibility and Effects of Newly Developed Balance Control Trainer for Mobility and Balance in Chronic Stroke Patients: A Randomized Controlled Trial
- Affiliations
-
- 1Department of Rehabilitation Medicine, Kyung-pook National University College of Medicine, Daegu 700-721, Korea. teeed0522@hanmail.net
- 2Department of Rehabilitation Medicine, Dae-gu Fatima Hospital, Daegu 701-600, Korea.
- KMID: 2266723
- DOI: http://doi.org/10.5535/arm.2012.36.4.521
Abstract
OBJECTIVE
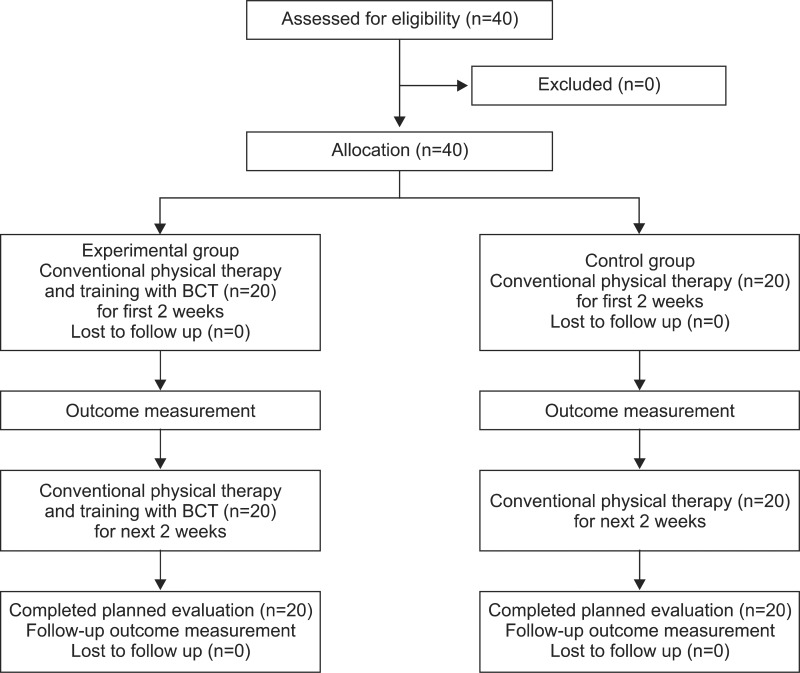
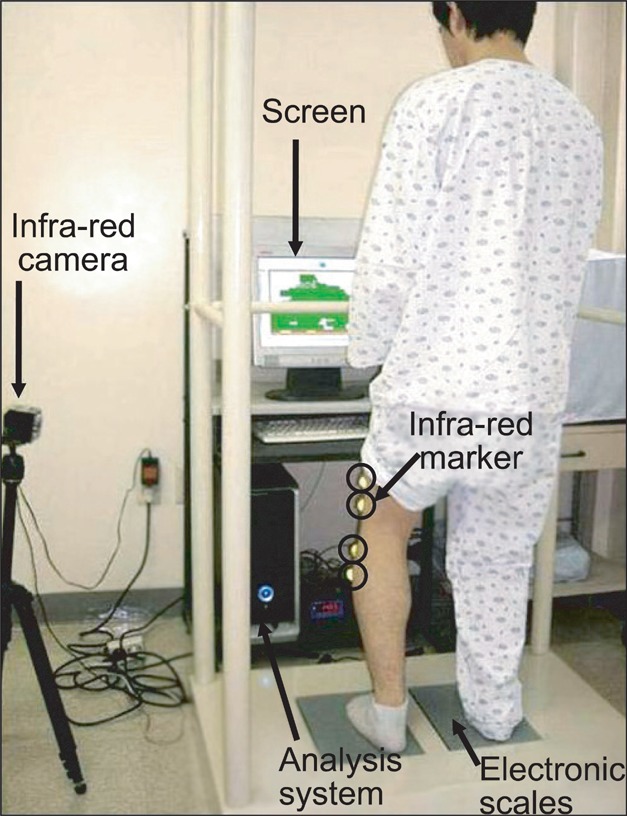
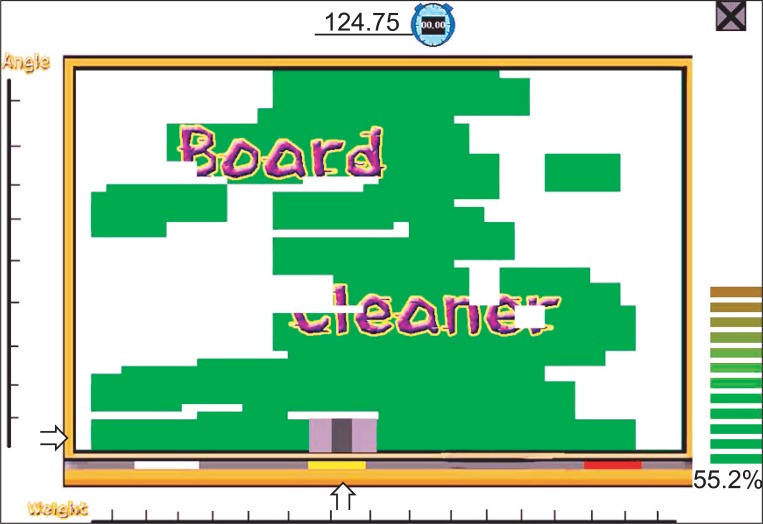
To investigate the feasibility and effects of balance training with a newly developed Balance Control Trainer (BCT) that applied the concept of vertical movement for the improvements of mobility and balance in chronic stroke patients. METHOD: Forty chronic stroke patients were randomly assigned to an experimental or a control group. The experimental group (n=20) underwent training with a BCT for 20 minutes a day, 5 days a week for 4 weeks, in addition to concurrent conventional physical therapy. The control group (n=20) underwent only conventional therapy for 4 weeks. All participants were assessed by: the Functional Ambulation Categories (FAC), 10-meter Walking Test (10mWT), Timed Up and Go test (TUG), Berg Balance Scale (BBS), Korean Modified Barthel Index (MBI), and Manual Muscle Test (MMT) before training, and at 2 and 4 weeks of training.
RESULTS
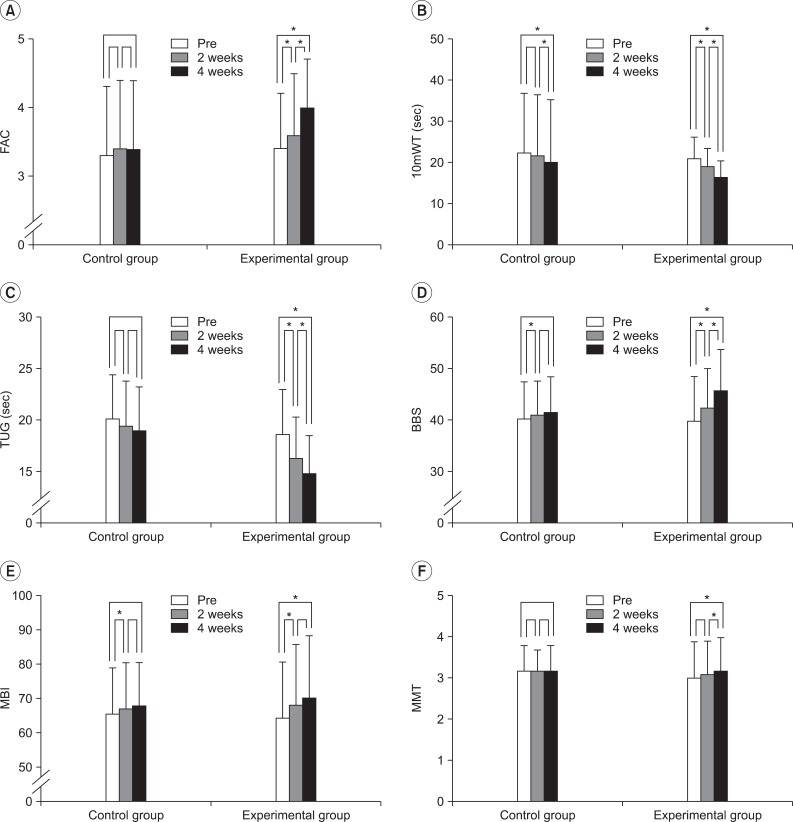
There were statistically significant improvements in all parameters except knee extensor power at 2 weeks of treatment, and in all parameters except MBI which showed further statistically significant progress in the experimental group over the next two weeks (p<0.05). Statistically significant improvements on all measurements were observed in the experimental group after 4 weeks total. Comparing the two groups at 2 and 4 weeks of training respectively, 10mWT, TUG, and BBS showed statistically more significant improvements in the experimental group (p<0.05).
CONCLUSION
Balance training with a newly developed BCT is feasible and may be an effective tool to improve balance and gait in ambulatory chronic stroke patients. Furthermore, it may provide additional benefits when used in conjunction with conventional therapies.
Figure
Cited by 2 articles
-
Effects of Balance Control Training on Functional Outcomes in Subacute Hemiparetic Stroke Patients
Jin Seok Huh, Yang-Soo Lee, Chul-Hyun Kim, Yu-Sun Min, Min-Gu Kang, Tae-Du Jung
Ann Rehabil Med. 2015;39(6):995-1001. doi: 10.5535/arm.2015.39.6.995.Balance Assessment in Subacute Stroke Patients Using the Balance Control Trainer (BalPro)
Jin Won Song, Jong Min Kim, Youn Soo Cheong, Yang-Soo Lee, Seong Min Chun, Yu-Sun Min, Tae-Du Jung
Ann Rehabil Med. 2017;41(2):188-196. doi: 10.5535/arm.2017.41.2.188.
Reference
-
1. Brandstater ME, de Bruin H, Gowland C, Clark BM. Hemiplegic gait: analysis of temporal variables. Arch Phys Med Rehabil. 1983; 64:583–587. PMID: 6661021.2. Skilbeck CE, Wade DT, Hewer RL, Wood VA. Recovery after stroke. J Neurol Neurosurg Psychiatry. 1983; 46:5–8. PMID: 6842200.
Article3. Wade DT, Wood VA, Hewer RL. Recovery after stroke--the first 3 months. J Neurol Neurosurg Psychiatry. 1985; 48:7–13. PMID: 3973623.
Article4. Bobath B. Adult hemiplegia: evaluation and treatment. 1990. 3rd ed. London: Butterworth-Heinemann;p. 70–160.5. Lorish TR, Sandin KJ, Roth EJ, Noll SF. Stroke rehabilitation. 3. Rehabilitation evaluation and management. Arch Phys Med Rehabil. 1994; 75:S47–S51. PMID: 7514395.6. Hesse S, Bertelt C, Jahnke MT, Schaffrin A, Baake P, Malezic M, Mauritz KH. Treadmill training with partial body weight support compared with physiotherapy in nonambulatory hemiparetic patients. Stroke. 1995; 26:976–981. PMID: 7762049.
Article7. Hesse S, Bertelt C, Schaffrin A, Malezic M, Mauritz KH. Restoration of gait in nonambulatory hemiparetic patients by treadmill training with partial body-weight support. Arch Phys Med Rehabil. 1994; 75:1087–1093. PMID: 7944913.
Article8. Patton J, Brown DA, Peshkin M, Santos-Munne JJ, Makhlin A, Lewis E, Colgate EJ, Schwandt D. KineAssist: design and development of a robotic overground gait and balance therapy device. Top Stroke Rehabil. 2008; 15:131–139. PMID: 18430678.
Article9. Mayr A, Kofler M, Quirbach E, Matzak H, Frohlich K, Saltuari L. Prospective, blinded, randomized crossover study of gait rehabilitation in stroke patients using the Lokomat gait orthosis. Neurorehabil Neural Repair. 2007; 21:307–314. PMID: 17476001.
Article10. Husemann B, Muller F, Krewer C, Heller S, Koenig E. Effects of locomotion training with assistance of a robot-driven gait orthosis in hemiparetic patients after stroke: a randomized controlled pilot study. Stroke. 2007; 38:349–354. PMID: 17204680.11. Chen IC, Cheng PT, Chen CL, Chen SC, Chung CY, Yeh TH. Effects of balance training on hemiplegic stroke patients. Chang Gung Med J. 2002; 25:583–590. PMID: 12479619.12. Nichols DS. Balance retraining after stroke using force platform biofeedback. Phys Ther. 1997; 77:553–558. PMID: 9149764.
Article13. Liston RA, Brouwer BJ. Reliability and validity of measures obtained from stroke patients using the Balance Master. Arch Phys Med Rehabil. 1996; 77:425–430. PMID: 8629916.
Article14. Matjacic Z, Hesse S, Sinkjaer T. BalanceReTrainer: a new standing-balance training apparatus and methods applied to a chronic hemiparetic subject with a neglect syndrome. NeuroRehabilitation. 2003; 18:251–259. PMID: 14530590.15. Kim CH, Byun SD, Shin OS, Kim TG, Kwon SM, Noh JH, Lee YS, Jung SK. Effects of the balance control of the affected lower extremity on balance and gait in hemiparetic patients. J Korean Acad Rehabil Med. 2008; 32:394–399.16. Yelnik A, Bonan I. Clinical tools for assessing balance disorders. Neurophysiol Clin. 2008; 38:439–445. PMID: 19026963.
Article17. Jung HY, Park JH, Shim JJ, Kim MJ, Hwang MR, Kim SH. Reliability test of Korean version of Berg balance scale. J Korean Acad Rehabil Med. 2006; 30:611–618.18. Mehrholz J, Wagner K, Rutte K, Meissner D, Pohl M. Predictive validity and responsiveness of the functional ambulation category in hemiparetic patients after stroke. Arch Phys Med Rehabil. 2007; 88:1314–1319. PMID: 17908575.
Article19. Pohl PS, Duncan PW, Perera S, Liu W, Lai SM, Studenski S, Long J. Influence of stroke-related impairments on performance in 6-minute walk test. J Rehabil Res Dev. 2002; 39:439–444. PMID: 17638141.20. Podsiadlo D, Richardson S. The timed "Up & Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991; 39:142–148. PMID: 1991946.21. Jung HY, Park BK, Shin HS, Kang YK, Pyun SB, Paik NJ, Kim SH, Kim TH, Han TR. Development of the Korean version of modified Barthel index (K-MBI): Multicenter study for subjects with stroke. J Korean Acad Rehabil Med. 2007; 31:283–297.22. Winstein CJ. Knowledge of results and motor learning--implications for physical therapy. Phys Ther. 1991; 71:140–149. PMID: 1989009.
Article23. Dickstein R, Nissan M, Pillar T, Scheer D. Foot-ground pressure pattern of standing hemiplegic patients. Major characteristics and patterns of improvement. Phys Ther. 1984; 64:19–12. PMID: 6691049.24. de Haart M, Geurts AC, Dault MC, Nienhuis B, Duysens J. Restoration of weight-shifting capacity in patients with postacute stroke: a rehabilitation cohort study. Arch Phys Med Rehabil. 2005; 86:755–762. PMID: 15827928.
Article25. Winstein CJ, Gardner ER, McNeal DR, Barto PS, Nicholson DE. Standing balance training: effect on balance and locomotion in hemiparetic adults. Arch Phys Med Rehabil. 1989; 70:755–762. PMID: 2802955.26. Moseley AM, Stark A, Cameron ID, Pollock A. Treadmill training and body weight support for walking after stroke. Cochrane Database Syst Rev. 2005; CD002840. PMID: 16235304.
Article27. Mehrholz J, Werner C, Kugler J, Pohl M. Electromechanical-assisted training for walking after stroke. Cochrane Database Syst Rev. 2007; CD006185. PMID: 17943893.
Article28. Yavuzer G, Eser F, Karakus D, Karaoglan B, Stam HJ. The effects of balance training on gait late after stroke: a randomized controlled trial. Clin Rehabil. 2006; 20:960–969. PMID: 17065539.
Article29. Eser F, Yavuzer G, Karakus D, Karaoglan B. The effect of balance training on motor recovery and ambulation after stroke: a randomized controlled trial. Eur J Phys Rehabil Med. 2008; 44:19–25. PMID: 18385624.30. Barclay-Goddard R, Stevenson T, Poluha W, Moffatt ME, Taback SP. Force platform feedback for standing balance training after stroke. Cochrane Database Syst Rev. 2004; CD004129. PMID: 15495079.
Article31. Richards CL, Malouin F, Wood-Dauphinee S, Williams JI, Bouchard JP, Brunet D. Task-specific physical therapy for optimization of gait recovery in acute stroke patients. Arch Phys Med Rehabil. 1993; 74:612–620. PMID: 8503751.
Article32. Lee MY, Wong MK, Tang FT, Cheng PT, Lin PS. Comparison of balance responses and motor patterns during sit-to-stand task with functional mobility in stroke patients. Am J Phys Med Rehabil. 1997; 76:401–410. PMID: 9354495.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of 3-Dimensional Lumbar Stabilization Training for Balance in Chronic Hemiplegic Stroke Patients: A Randomized Controlled Trial
- Effects of the Balance Control Training in Chronic Hemiplegic Stroke Patients
- The Effects of Additional Balance Training in Subacute Hemiplegic Stroke Patients
- Effects of the Balance Control of the Affected Lower Extremityon Balance and Gait in Hemiparetic Patients
- Effects of Balance Control Training on Functional Outcomes in Subacute Hemiparetic Stroke Patients