Ann Dermatol.
2014 Oct;26(5):621-623. 10.5021/ad.2014.26.5.621.
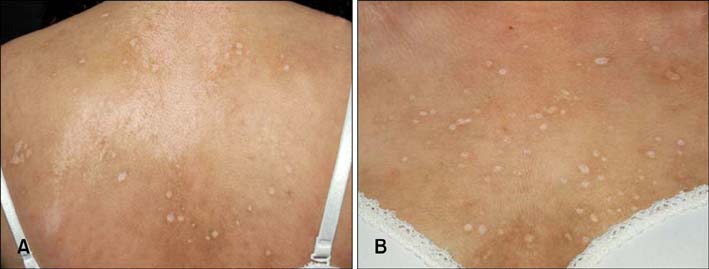
Eruptive Anetoderma in a Patient with Systemic Lupus Erythematosus
- Affiliations
-
- 1Department of Dermatology, Chungnam National University School of Medicine, Daejeon, Korea. resina20@cnu.ac.kr
- KMID: 2265499
- DOI: http://doi.org/10.5021/ad.2014.26.5.621
Abstract
- Anetoderma is a rare cutaneous disorder characterized by a loss of normal elastic tissue that presents clinically as atrophic patches located mainly on the upper trunk. Recent studies suggest immunological mechanisms may play a role in this process. Furthermore, a secondary form of macular atrophy occurs in the course of infectious diseases (e.g. syphilis and tuberculosis) and autoimmune disease (e.g. systemic lupus erythematosus [SLE]). Here, we report the case of a 20-year-old woman previously diagnosed with SLE, who presented with numerous well-circumscribed atrophic macules on the face and upper trunk. Histopathological examination showed decreased elastic tissues in the reticular dermis and mononuclear cells adhering to elastic fibers, consistent with anetoderma. Thus, the eruptive anetoderma localized widely on the face and upper trunk may have been caused by an autoimmune response of SLE.
Keyword
MeSH Terms
Figure
Reference
-
1. Venencie PY, Winkelmann RK. Monoclonal antibody studies in the skin lesions of patients with anetoderma. Arch Dermatol. 1985; 121:747–749.
Article2. Hodak E, Shamai-Lubovitz O, David M, Hazaz B, Katzenelson-Weissman V, Lahav M, et al. Immunologic abnormalities associated with primary anetoderma. Arch Dermatol. 1992; 128:799–803.
Article3. Romaní J, Pérez F, Llobet M, Planagumá M, Pujol RM. Anetoderma associated with antiphospholipid antibodies: case report and review of the literature. J Eur Acad Dermatol Venereol. 2001; 15:175–178.
Article4. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ. Fitzpatrick's dermatology in general medicine. 7th ed. New York: McGraw-Hill;2008. p. 547p. 567–568.5. Schmitt D, Thivolet J, Perrot H. Ultrastructural study of the cutaneous elastic fibres in lupus erythematosus. Br J Dermatol. 1972; 87:355–360.
Article6. Sparsa A, Piette JC, Wechsler B, Amoura Z, Francès C. Anetoderma and its prothrombotic abnormalities. J Am Acad Dermatol. 2003; 49:1008–1012.
Article7. Hodak E, David M. Primary anetoderma and antiphospholipid antibodies--review of the literature. Clin Rev Allergy Immunol. 2007; 32:162–166.
Article8. Hodak E, Shamai-Lubovitz O, David M, Hazaz B, Lahav M, Sandbank M. Primary anetoderma associated with a wide spectrum of autoimmune abnormalities. J Am Acad Dermatol. 1991; 25:415–418.
Article9. Montilla C, Alarcón-Segovia D. Anetoderma in systemic lupus erythematosus: relationship to antiphospholipid antibodies. Lupus. 2000; 9:545–547.
Article10. Lindstrom J, Smith KJ, Skelton HG, Redfield R, Alving BM, Wagner KF, et al. Increased anticardiolipin antibodies associated with the development of anetoderma in HIV-1 disease. Military Medical Consortium for the Advancement of Retroviral research (MMCARR). Int J Dermatol. 1995; 34:408–415.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple Eruptive Dermatofibromas in a Patient with Systemic Lupus Erythematosus and Juvenile Rheumatoid Arthritis
- A Case of Multiple Eruptive Dermatofibromas in a Patient with Systemic Lupus Erythematosus
- A Case of Transverse Myelitis as a First Manifestation of Systemic Lupus Erythematosus
- A Ruptured Aneurysm in a Patient with Systemic Lupus Erythematosus: Case Report
- A Case Of Systemic Lupus Erythematosus Associated With Hyperthyroidism And Severe Retinopathy