Allergy Asthma Immunol Res.
2014 Jul;6(4):310-315. 10.4168/aair.2014.6.4.310.
Influence of Chronic Sinusitis and Nasal Polyp on the Lower Airway of Subjects Without Lower Airway Diseases
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. shcho@snu.ac.kr
- 2Institute of Allergy and Clinical Immunology, Seoul National University Medical Research Center, Seoul, Korea.
- 3Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- 4Department of Radiology, Seoul National University College of Medicine, Seoul, Korea.
- 5Seoul National University Hospital Healthcare System Gangnam Center, Seoul, Korea.
- KMID: 2260211
- DOI: http://doi.org/10.4168/aair.2014.6.4.310
Abstract
- PURPOSE
Upper and lower respiratory tract pathologies are believed to be interrelated; however, the impact of upper airway inflammation on lung function in subjects without lung disease has not been evaluated. This study investigated the association of CT finding suggesting chronic sinusitis and lung function in healthy subjects without lung disease.
METHODS
This was a retrospective study of prospectively collected data from 284 subjects who underwent a pulmonary function test, bronchial provocation test, rhinoscopy, and osteomeatal unit computed tomography offered as a private health check-up option.
RESULTS
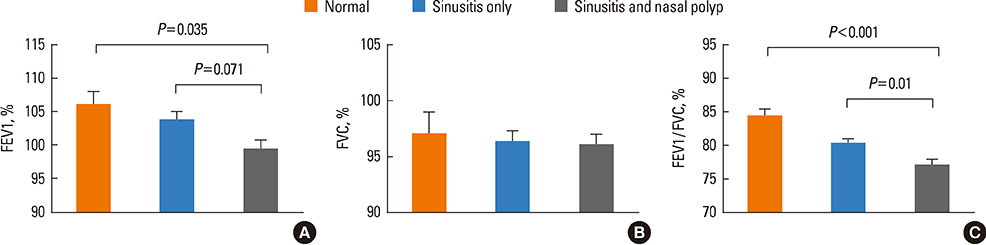
CT findings showed that the sinusitis group had a significantly lower FEV1/FVC ratio than subjects without sinusitis finding (78.62% vs 84.19%, P=0.019). Among the sinusitis group, subjects classified by CT findings as the extensive disease group had a slightly lower FEV1/FVC than those of the limited disease group (76.6% vs 79.5%, P=0.014) and the associations were independent of the presence of airway hyperresponsiveness. The subjects with nasal polyp had also lower FEV1 and FEV1/FVC than subjects without nasal polyp (FEV1: 100.0% vs 103.6%, P=0.045, FEV1/FVC: 77.4% vs 80.0%, P=0.005).
CONCLUSIONS
CT findings suggesting chronic sinusitis and nasal polyp were associated with subclinical lower airway flow limitation even in the absence of underlying lung disease.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The Lung Function Impairment in Non-Atopic Patients With Chronic Rhinosinusitis and Its Correlation Analysis
Linghao Zhang, Lu Zhang, Chun-Hong Zhang, Xiao-Bi Fang, Zhen-Xiao Huang, Qing-Yuan Shi, Li-Ping Wu, Peng Wu, Zhen-Zhen Wang, Zhi-Su Liao
Clin Exp Otorhinolaryngol. 2016;9(4):339-345. doi: 10.21053/ceo.2015.01641.
Reference
-
1. Fokkens W, Lund V, Mullol J. European position paper on rhinosinusitis and nasal polyps group. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2008; 43:317–320.2. Ikeda K, Oshima T, Furukawa M, Katori Y, Shimomura A, Takasaka T, Maruoka S. Restoration of the mucociliary clearance of the maxillary sinus after endoscopic sinus surgery. J Allergy Clin Immunol. 1997; 99:48–52.3. Meltzer EO, Hamilos DL, Hadley JA, Lanza DC, Marple BF, Nicklas RA, Bachert C, Baraniuk J, Baroody FM, Benninger MS, Brook I, Chowdhury BA, Druce HM, Durham S, Ferguson B, Gwaltney JM Jr, Kaliner M, Kennedy DW, Lund V, Naclerio R, Pawankar R, Piccirillo JF, Rohane P, Simon R, Slavin RG, Togias A, Wald ER, Zinreich SJ. American Academy of Otolaryngic Allergy, Asthma and Immunology. American Academy of Otolaryngic Allergy. American Academy of Otolaryngology-Head and Neck Surgery. American College of Allergy, Asthma and Immunology. American Rhinologic Society. Rhinosinusitis: Establishing definitions for clinical research and patient care. Otolaryngol Head Neck Surg. 2004; 131:S1–S62.4. Benitez P, Alobid I, de Haro J, Berenguer J, Bernal-Sprekelsen M, Pujols L, Picado C, Mullol J. A short course of oral prednisone followed by intranasal budesonide is an effective treatment of severe nasal polyps. Laryngoscope. 2006; 116:770–775.5. Zimmerman B. Clinical experience with the measurement of ECP: usefulness in the management of children with asthma. Clin Exp Allergy. 1993; 23:Suppl 2. 8–12.6. Guilemany JM, Angrill J, Alobid I, Centellas S, Prades E, Roca J, Pujols L, Bernal-Sprekelsen M, Picado C, Mullol J. United airways: the impact of chronic rhinosinusitis and nasal polyps in bronchiectasic patient's quality of life. Allergy. 2009; 64:1524–1529.7. Kelemence A, Abadoglu O, Gumus C, Berk S, Epozturk K, Akkurt I. The frequency of chronic rhinosinusitis/nasal polyp in COPD and its effect on the severity of COPD. COPD. 2011; 8:8–12.8. Leynaert B, Neukirch F, Demoly P, Bousquet J. Epidemiologic evidence for asthma and rhinitis comorbidity. J Allergy Clin Immunol. 2000; 106:S201–S205.9. Hurst JR, Wilkinson TM, Donaldson GC, Wedzicha JA. Upper airway symptoms and quality of life in chronic obstructive pulmonary disease (COPD). Respir Med. 2004; 98:767–770.10. Proimos E, Papadakis CE, Chimona TS, Kiagiadaki D, Ferekidis E, Yiotakis J. The effect of functional endoscopic sinus surgery on patients with asthma and CRS with nasal polyps. Rhinology. 2010; 48:331–338.11. Tsao CH, Chen LC, Yeh KW, Huang JL. Concomitant chronic sinusitis treatment in children with mild asthma: the effect on bronchial hyperresponsiveness. Chest. 2003; 123:757–764.12. Bresciani M, Paradis L, Des Roches A, Vernhet H, Vachier I, Godard P, Bousquet J, Chanez P. Rhinosinusitis in severe asthma. J Allergy Clin Immunol. 2001; 107:73–80.13. Hens G, Vanaudenaerde BM, Bullens DM, Piessens M, Decramer M, Dupont LJ, Ceuppens JL, Hellings PW. Sinonasal pathology in nonallergic asthma and COPD: 'united airway disease' beyond the scope of allergy. Allergy. 2008; 63:261–267.14. Kim YK, Kim SH, Tak YJ, Jee YK, Lee BJ, Kim SH, Park HW, Jung JW, Bahn JW, Chang YS, Choi DC, Chang SI, Min KU, Kim YY, Cho SH. High prevalence of current asthma and active smoking effect among the elderly. Clin Exp Allergy. 2002; 32:1706–1712.15. Newman LJ, Platts-Mills TA, Phillips CD, Hazen KC, Gross CW. Chronic sinusitis. Relationship of computed tomographic findings to allergy, asthma, and eosinophilia. JAMA. 1994; 271:363–367.16. Blanton PL, Biggs NL. Eighteen hundred years of controversy: the paranasal sinuses. Am J Anat. 1969; 124:135–147.17. Dixon AE, Kaminsky DA, Holbrook JT, Wise RA, Shade DM, Irvin CG. Allergic rhinitis and sinusitis in asthma: differential effects on symptoms and pulmonary function. Chest. 2006; 130:429–435.18. Bourdin A, Gras D, Vachier I, Chanez P. Upper airway x 1: allergic rhinitis and asthma: united disease through epithelial cells. Thorax. 2009; 64:999–1004.19. Copilevitz C, Slavin R. Sinusitis and asthma. In : Kaliner MA, editor. Current review of asthma. Philadelphia (PA): Current Medicine LLC;2003. p. 61–65.20. Rolla G, Colagrande P, Scappaticci E, Bottomicca F, Magnano M, Brussino L, Dutto L, Bucca C. Damage of the pharyngeal mucosa and hyperresponsiveness of airway in sinusitis. J Allergy Clin Immunol. 1997; 100:52–57.21. Georgitis JW, Matthews BL, Stone B. Chronic sinusitis: characterization of cellular influx and inflammatory mediators in sinus lavage fluid. Int Arch Allergy Immunol. 1995; 106:416–421.22. Braunstahl GJ, Overbeek SE, Kleinjan A, Prins JB, Hoogsteden HC, Fokkens WJ. Nasal allergen provocation induces adhesion molecule expression and tissue eosinophilia in upper and lower airways. J Allergy Clin Immunol. 2001; 107:469–476.23. Saito H, Howie K, Wattie J, Denburg A, Ellis R, Inman MD, Denburg JA. Allergen-induced murine upper airway inflammation: local and systemic changes in murine experimental allergic rhinitis. Immunology. 2001; 104:226–234.24. Beeh KM, Beier J, Kornmann O, Meier C, Taeumer T, Buhl R. A single nasal allergen challenge increases induced sputum inflammatory markers in non-asthmatic subjects with seasonal allergic rhinitis: correlation with plasma interleukin-5. Clin Exp Allergy. 2003; 33:475–482.25. Griffin MP, McFadden ER Jr, Ingram RH Jr. Airway cooling in asthmatic and nonasthmatic subjects during nasal and oral breathing. J Allergy Clin Immunol. 1982; 69:354–359.26. Bhattacharyya N. Clinical and symptom criteria for the accurate diagnosis of chronic rhinosinusitis. Laryngoscope. 2006; 116:1–22.27. Osguthorpe JD. Adult rhinosinusitis: diagnosis and management. Am Fam Physician. 2001; 63:69–76.28. Kaliner MA, Osguthorpe JD, Fireman P, Anon J, Georgitis J, Davis ML, Naclerio R, Kennedy D. Sinusitis: bench to bedside. Current findings, future directions. Otolaryngol Head Neck Surg. 1997; 116:S1–S20.29. Settipane RA. Complications of allergic rhinitis. Allergy Asthma Proc. 1999; 20:209–213.30. ten Brinke A, Grootendorst DC, Schmidt JT, De Bruïne FT, van Buchem MA, Sterk PJ, Rabe KF, Bel EH. Chronic sinusitis in severe asthma is related to sputum eosinophilia. J Allergy Clin Immunol. 2002; 109:621–626.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Coexisting Upper Airway Inflammation in Chronic Obstructive Pulmonary Disease: A Review of the Literature
- The Effect of Lower Airway Disease on the Severity of Chronic Rhinosinusitis
- Unified Airway in ENT Field
- Detection of Staphylococcus Aureus Exotoxins(SEA, TSST-1) in Nasal Polyp with Chronic Rhinosinusitis Patients
- Allergic rhinitis, sinusitis and asthma: evidence for respiratory system integration