Korean J Hepatobiliary Pancreat Surg.
2016 May;20(2):81-84. 10.14701/kjhbps.2016.20.2.81.
Management of portal hypertension derived from uncommon causes
- Affiliations
-
- 1Department of Hepatobiliary and Pancreatic Surgery, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. kskim88@yuhs.ac
- 2Department of Radiology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2243020
- DOI: http://doi.org/10.14701/kjhbps.2016.20.2.81
Abstract
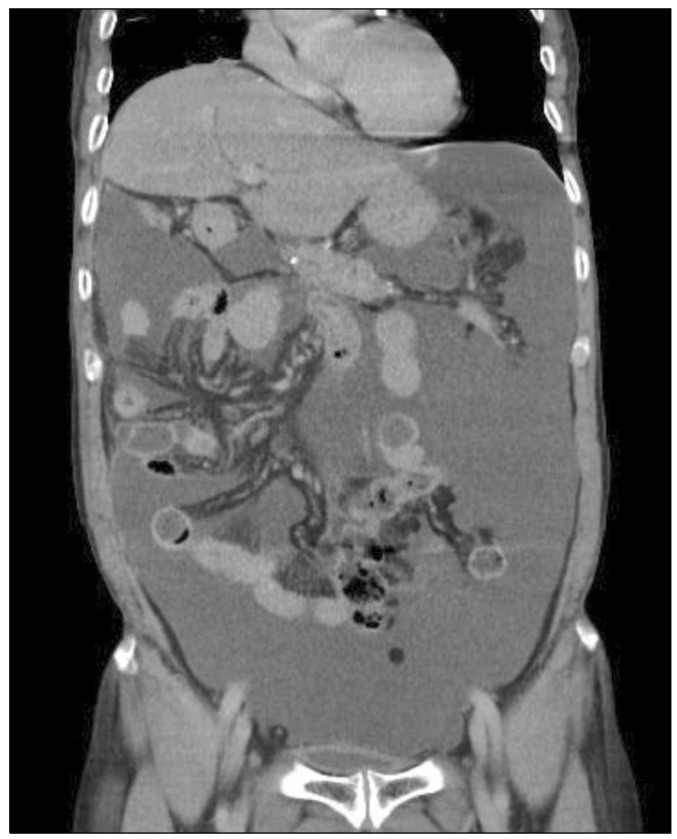
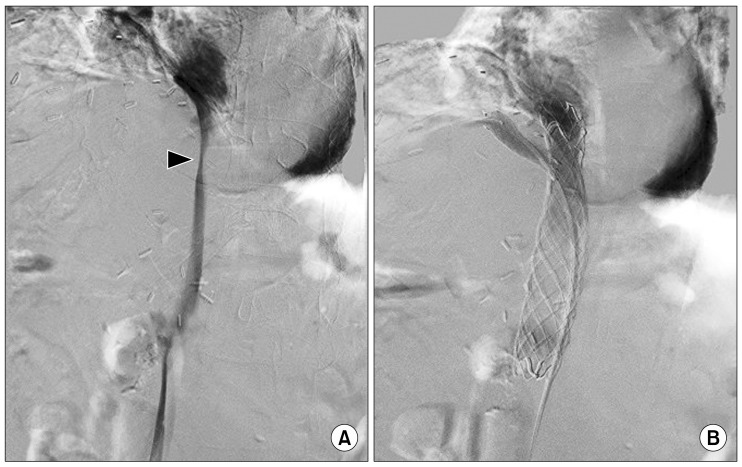
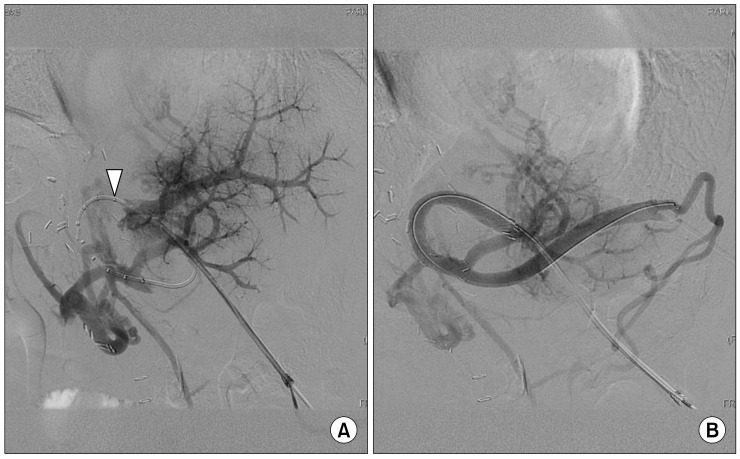
- Portal hypertension can arise from any condition interfering with normal blood flow at any level within the portal system. Herein, we presented two uncommon cases of the portal hypertension and its treatment with brief literature review. A 71-year-old man who underwent right hemihepatectomy revealed a tumor recurrence adjacent to the inferior vena cava (IVC). After radiofrequency ablation (RFA) with lymph node dissection, he was referred for abdominal distension. The abdomen computed tomography scan showed severe ascites with a narrowing middle hepatic vein (MHV) and IVC around the RFA site. After insertion of two stents at the IVC and MHV, the ascites disappeared. Another 73-year-old man underwent right trisectionectomy of liver and segmental resection of the portal vein (PV). After operation, he underwent conservative management due to continuous abdominal ascites. The abdomen computed tomography scan showed severe ascites with obliteration of the left PV. After insertion of stent, the ascites disappeared. A decrease of the pressure gradient between the PV and IVC is one of the important treatment strategies for portal hypertension. Vascular stent is useful in the reduction of pressure gradient and thus, can be a treatment option for portal hypertension.
Keyword
MeSH Terms
Figure
Reference
-
1. Bosch J, Groszmann RJ, Shah VH. Evolution in the understanding of the pathophysiological basis of portal hypertension: How changes in paradigm are leading to successful new treatments. J Hepatol. 2015; 62(1 Suppl):S121–S130. PMID: 25920081.
Article2. Khanna R, Sarin SK. Non-cirrhotic portal hypertension - diagnosis and management. J Hepatol. 2014; 60:421–441. PMID: 23978714.
Article3. Sanyal AJ, Bosch J, Blei A, Arroyo V. Portal hypertension and its complications. Gastroenterology. 2008; 134:1715–1728. PMID: 18471549.
Article4. Bogin V, Marcos A, Shaw-Stiffel T. Budd-Chiari syndrome: in evolution. Eur J Gastroenterol Hepatol. 2005; 17:33–35. PMID: 15647637.5. Bayraktar UD, Seren S, Bayraktar Y. Hepatic venous outflow obstruction: three similar syndromes. World J Gastroenterol. 2007; 13:1912–1927. PMID: 17461490.
Article6. Akahane M, Koga H, Kato N, Yamada H, Uozumi K, Tateishi R, et al. Complications of percutaneous radiofrequency ablation for hepato-cellular carcinoma: imaging spectrum and management. Radiographics. 2005; 25(Suppl 1):S57–S68. PMID: 16227497.
Article7. Lu DS, Raman SS, Vodopich DJ, Wang M, Sayre J, Lassman C. Effect of vessel size on creation of hepatic radiofrequency lesions in pigs: assessment of the "heat sink" effect. AJR Am J Roentgenol. 2002; 178:47–51. PMID: 11756085.8. Parikh S, Shah R, Kapoor P. Portal vein thrombosis. Am J Med. 2010; 123:111–119. PMID: 20103016.
Article9. Wang J, Yang W, Huang Q, Gao K, Wei B, Zhai R, et al. Interventional treatment for portal venous occlusion after liver transplantation: long-term follow-up results. Medicine (Baltimore). 2015; 94:e356. PMID: 25634164.10. Woodrum DA, Bjarnason H, Andrews JC. Portal vein venoplasty and stent placement in the nontransplant population. J Vasc Interv Radiol. 2009; 20:593–599. PMID: 19339200.
Article11. Yamakado K, Nakatsuka A, Tanaka N, Fujii A, Isaji S, Kawarada Y, et al. Portal venous stent placement in patients with pancreatic and biliary neoplasms invading portal veins and causing portal hypertension: initial experience. Radiology. 2001; 220:150–156. PMID: 11425988.
Article12. Garcia-Tsao G, Bosch J. Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med. 2010; 362:823–832. PMID: 20200386.
Article13. Zhou ZQ, Lee JH, Song KB, Hwang JW, Kim SC, Lee YJ, et al. Clinical usefulness of portal venous stent in hepatobiliary pancreatic cancers. ANZ J Surg. 2014; 84:346–352. PMID: 23421858.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Portal hypertension in children
- Diagnosis and Management of Esophageal and Gastric Variceal Bleeding: Focused on 2019 KASL Clinical Practice Guidelines for Liver Cirrhosis
- Assessment and Current Treatment of Portal Hypertension
- Experimental Animal Models of Portal Hypertension
- Congenital Absence of the Portal Vein Presenting as Pulmonary Hypertension