Korean J Hepatobiliary Pancreat Surg.
2016 May;20(2):53-60. 10.14701/kjhbps.2016.20.2.53.
Safe laparoscopic clearance of the common bile duct in emergently admitted patients with choledocholithiasis and cholangitis
- Affiliations
-
- 1Department of General and Emergency Surgery, Riga East University Hospital, Riga, Latvia. kristofss@inbox.lv
- KMID: 2243015
- DOI: http://doi.org/10.14701/kjhbps.2016.20.2.53
Abstract
- BACKGROUNDS/AIMS
Laparoscopic treatment of patients with choledocholithiasis and cholangitis is challenging due to mandatory recovery of the biliary drainage and clearance of the common bile duct (CBD). The aim of our study was to assess postoperative course of cholangitis and biliary sepsis after laparoscopic clearance of the CBD in emergently admitted patients with choledocholithiasis and cholangitis.
METHODS
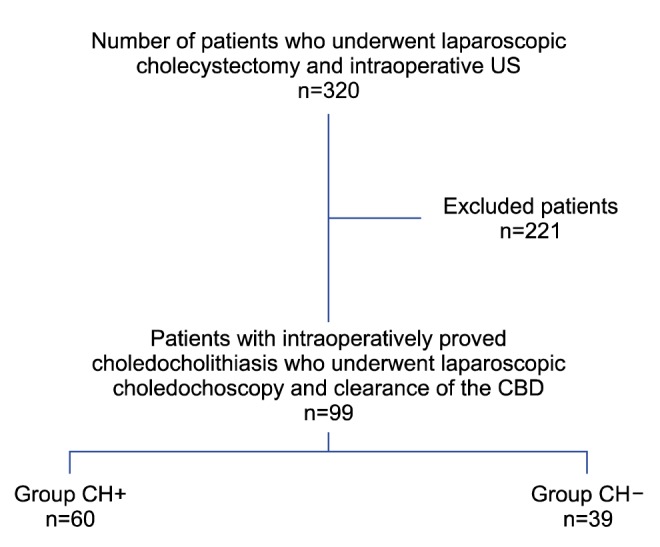
Emergently admitted patients who underwent laparoscopic clearance of the CBD were included prospectively and stratified in 2 groups i.e., cholangitis positive (CH+) or negative (CH-) group. Patient demographics, comorbidities, preoperative imaging data, inflammatory response, surgical intervention, complication rate and outcomes were compared between groups.
RESULTS
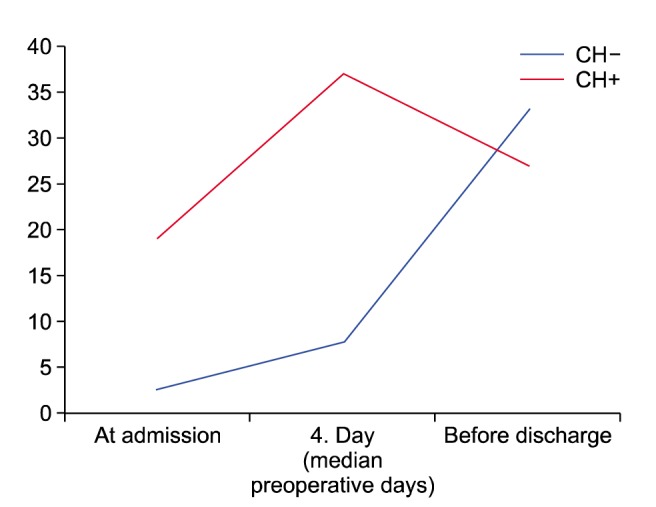
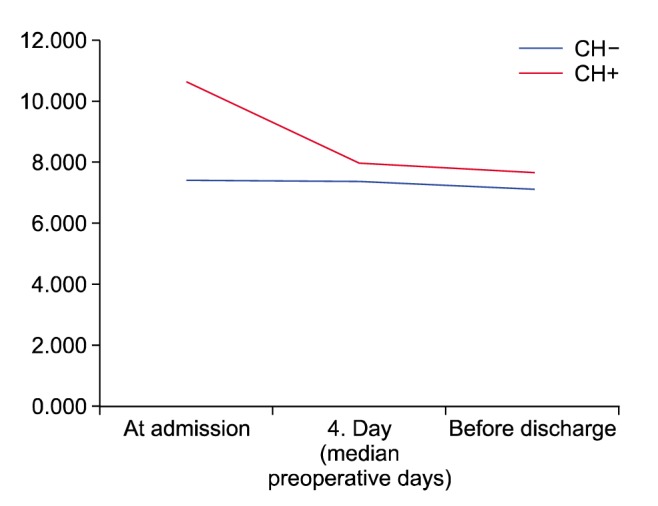
Ninety-nine of a total 320 patients underwent laparoscopic clearance of the CBD, of which, 60 belonged to the acute cholangitis group (CH+) and 39 to the cholangitis negative group (CH-). Interventions were done on average 4 days after admission, operation duration was 95-105 min, and the conversion rate was 3-7% without differences in the groups. Preoperative inflammatory response was markedly higher in the CH+ group. Inflammation signs on intraoperative choledochoscopy were more evident in patients with cholangitis. Postoperative inflammatory response did not differ between the groups. The overall complication rate was 8.3% and 5.1%, respectively. Laparoscopic clearance of the CBD resulted in 1 lethal case (CH+ group), resulting in 1% mortality rate and a similar 12-month readmission rate.
CONCLUSIONS
Single-stage laparoscopic intraoperative US and choledochoscopy-assisted clearance of the CBD is feasible in emergently admitted patients with choledocholithiasis and cholangitis.
Keyword
MeSH Terms
Figure
Reference
-
1. Freitas ML, Bell RL, Duffy AJ. Choledocholithiasis: evolving standards for diagnosis and management. World J Gastroenterol. 2006; 12:3162–3167. PMID: 16718834.
Article2. Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996; 335:909–918. PMID: 8782497.
Article3. Adler DG, Baron TH, Davila RE, Egan J, Hirota WK, Leighton JA, et al. ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas. Gastrointest Endosc. 2005; 62:1–8. PMID: 15990812.
Article4. Hublet A, Dili A, Lemaire J, Mansvelt B, Molle G, Bertrand C. Laparoscopic ultrasonography as a good alternative to intraoperative cholangiography (IOC) during laparoscopic cholecystectomy: results of prospective study. Acta Chir Belg. 2009; 109:312–316. PMID: 19943585.
Article5. Aziz O, Ashrafian H, Jones C, Harling L, Kumar S, Garas G, et al. Laparoscopic ultrasonography versus intra-operative cholangiogram for the detection of common bile duct stones during laparoscopic cholecystectomy: a meta-analysis of diagnostic accuracy. Int J Surg. 2014; 12:712–719. PMID: 24861544.
Article6. Takada T, Strasberg SM, Solomkin JS, Pitt HA, Gomi H, Yoshida M, et al. TG13: Updated Tokyo Guidelines for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2013; 20:1–7. PMID: 23307006.7. Kiriyama S, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Pitt HA, et al. TG13 guidelines for diagnosis and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2013; 20:24–34. PMID: 23307001.8. Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, et al. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013; 62:102–111. PMID: 23100216.
Article9. Sankar A, Johnson SR, Beattie WS, Tait G, Wijeysundera DN. Reliability of the American Society of Anesthesiologists physical status scale in clinical practice. Br J Anaesth. 2014; 113:424–432. PMID: 24727705.
Article10. Aronson WL, McAuliffe MS, Miller K. Variability in the American society of anesthesiologists physical status classification scale. AANA J. 2003; 71:265–274. PMID: 13677221.11. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013; 310:2191–2914. PMID: 24141714.12. Hallal AH, Amortegui JD, Jeroukhimov IM, Casillas J, Schulman CI, Manning RJ, et al. Magnetic resonance cholangiopancreatography accurately detects common bile duct stones in resolving gallstone pancreatitis. J Am Coll Surg. 2005; 200:869–875. PMID: 15922197.
Article13. Peng WK, Sheikh Z, Paterson-Brown S, Nixon SJ. Role of liver function tests in predicting common bile duct stones in acute calculous cholecystitis. Br J Surg. 2005; 92:1241–1247. PMID: 16078299.
Article14. Taylor AC, Little AF, Hennessy OF, Banting SW, Smith PJ, Desmond PV. Prospective assessment of magnetic resonance cholangiopancreatography for noninvasive imaging of the biliary tree. Gastrointest Endosc. 2002; 55:17–22. PMID: 11756908.
Article15. Topal B, Van de Moortel M, Fieuws S, Vanbeckevoort D, Van Steenbergen W, Aerts R, et al. The value of magnetic resonance cholangiopancreatography in predicting common bile duct stones in patients with gallstone disease. Br J Surg. 2003; 90:42–47. PMID: 12520573.
Article16. Akisik MF, Jennings SG, Aisen AM, Sherman S, Cote GA, Sandrasegaran K, et al. MRCP in patient care: a prospective survey of gastroenterologists. AJR Am J Roentgenol. 2013; 201:573–577. PMID: 23971448.
Article17. Chen W, Mo JJ, Lin L, Li CQ, Zhang JF. Diagnostic value of magnetic resonance cholangiopancreatography in choledocholithiasis. World J Gastroenterol. 2015; 21:3351–3360. PMID: 25805944.
Article18. Sinha R. Early laparoscopic cholecystectomy in acute biliary pancreatitis: the optimal choice? HPB (Oxford). 2008; 10:332–335. PMID: 18982148.
Article19. Costi R, Gnocchi A, Di Mario F, Sarli L. Diagnosis and management of choledocholithiasis in the golden age of imaging, endoscopy and laparoscopy. World J Gastroenterol. 2014; 20:13382–13401. PMID: 25309071.
Article20. Srinivasa S, Sammour T, McEntee B, Davis N, Hill AG. Selective use of magnetic resonance cholangiopancreatography in clinical practice may miss choledocholithiasis in gallstone pancreatitis. Can J Surg. 2010; 53:403–407. PMID: 21092433.21. Li P, Zhang Z, Li J, Jin L, Han W, Zhang J. Diagnostic value of magnetic resonance cholangiopancreatography for secondary common bile duct stones compared with laparoscopic trans-cystic common bile duct exploration. Med Sci Monit. 2014; 20:920–926. PMID: 24894946.
Article22. Sangrasi AK, Syed B, Memon AI, Laghari AA, Talpur KA, Qureshi JN. Laparoscopic cholecystectomy in acute gallstone pancreatitis in index hospital admission: feasibility and safety. Pak J Med Sci. 2014; 30:601–605. PMID: 24948988.
Article23. Cuschieri A, Lezoche E, Morino M, Croce E, Lacy A, Toouli J, et al. E.A.E.S. multicenter prospective randomized trial comparing two-stage vs single-stage management of patients with gallstone disease and ductal calculi. Surg Endosc. 1999; 13:952–957. PMID: 10526025.
Article24. Nealon WH, Bawduniak J, Walser EM. Appropriate timing of cholecystectomy in patients who present with moderate to severe gallstone-associated acute pancreatitis with peripancreatic fluid collections. Ann Surg. 2004; 239:741–749. PMID: 15166953.
Article25. Stone HH, Fabian TC, Dunlop WE. Gallstone pancreatitis: biliary tract pathology in relation to time of operation. Ann Surg. 1981; 194:305–312. PMID: 6168240.26. Tranter SE, Thompson MH. A prospective single-blinded controlled study comparing laparoscopic ultrasound of the common bile duct with operative cholangiography. Surg Endosc. 2003; 17:216–219. PMID: 12457223.
Article27. Metcalfe MS, Ong T, Bruening MH, Iswariah H, Wemyss-Holden SA, Maddern GJ. Is laparoscopic intraoperative cholangiogram a matter of routine? Am J Surg. 2004; 187:475–481. PMID: 15041494.
Article28. Santambrogio R, Bianchi P, Opocher E, Mantovani A, Schubert L, Ghelma F, et al. Intraoperative ultrasonography (IOUS) during laparoscopic cholecystectomy. Surg Endosc. 1996; 10:622–627. PMID: 8662399.
Article29. Overby DW, Apelgren KN, Richardson W, Fanelli R. Society of American Gastrointestinal and Endoscopic Surgeons. SAGES guidelines for the clinical application of laparoscopic biliary tract surgery. Surg Endosc. 2010; 24:2368–2386. PMID: 20706739.
Article30. Rhodes M, Sussman L, Cohen L, Lewis MP. Randomised trial of laparoscopic exploration of common bile duct versus postoperative endoscopic retrograde cholangiography for common bile duct stones. Lancet. 1998; 351:159–161. PMID: 9449869.
Article31. Naumowicz E, Białecki J, Kołomecki K. Results of treatment of patients with gallstone disease and ductal calculi by single-stage laparoscopic cholecystectomy and bile duct exploration. Wideochir Inne Tech Maloinwazyjne. 2014; 9:179–189. PMID: 25097684.
Article32. Bencini L, Tommasi C, Manetti R, Farsi M. Modern approach to cholecysto-choledocholithiasis. World J Gastrointest Endosc. 2014; 6:32–40. PMID: 24567790.
Article33. Koc B, Adas G, Karahan S. Use of laparoscopic common bile duct exploration for failed endoscopic bile duct stone extractions. Minerva Chir. 2014; 69:209–215. PMID: 24987968.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Surgery for Common Bile Duct Stone
- A Common Bile Duct Web Presenting with Obstructive Jaundice without Common Bile Duct Stone
- Ectopic Opening of the Common Bile Duct into the Duodenal Bulb: A Case Report
- Case Report of a Double Common Bile Duct with Gallstone Cholecystitis
- Surgical Clip Moved into the Extrahepatic Bile Duct after Laparoscopic Hepatectomy