Korean Circ J.
2007 Apr;37(4):148-153. 10.4070/kcj.2007.37.4.148.
The Usefulness of Intracoronary Electrocardiography during Primary Percutaneous Coronary Intervention in Patients with Acute Myocardial Infarction
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Yeungnam University Medical Center, Daegu, Korea. yjkim@med.yu.ac.kr
- 2Department of Internal Medicine, Dong Kang Hospital, Ulsan, Korea.
- KMID: 2227071
- DOI: http://doi.org/10.4070/kcj.2007.37.4.148
Abstract
-
BACKGROUND AND OBJECTIVES: Measurements obtained using an intracoronary electrocardiogram (IC-ECG) reflect the electrical activity in various regions of the myocardium. This technique can be easily used in the catheterization laboratory during percutaneous coronary intervention (PCI) procedures. Furthermore, IC-ECG could be used to evaluate myocardial viability in patients with acute myocardial infarction (AMI). The aim of this study was to evaluate the usefulness of IC-ECG in predicting the microvascular integrity and late improvement of left ventricular (LV) function after primary PCI in patients with AMI.
SUBJECTS AND METHODS
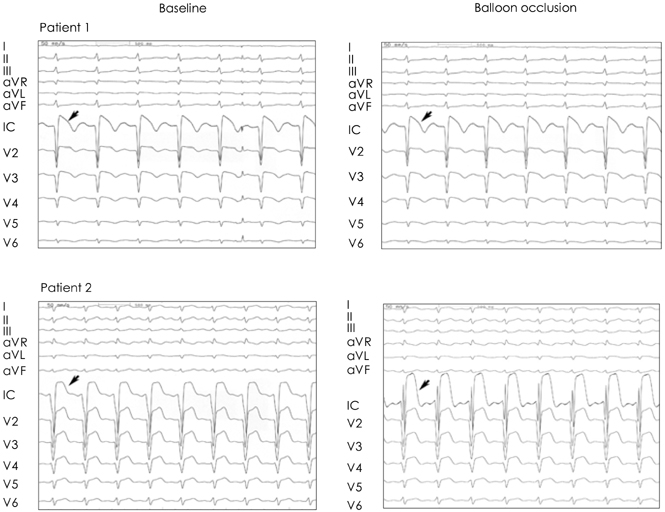
A total of 78 patients (62 male, 16 female) who underwent primary PCI with stent implantation were enrolled in this study. After the implantation of the stent, IC-ECG was recorded from the tip of an insulated angioplasty guidewire before and after balloon occlusion of the infarct-related artery. The IC-ECG was obtained from the inferior and inferolateral areas in inferior wall MI, or apex and apical anterior wall regions in anterior wall MI. Significant ST segment elevation was defined as a further ST segment elevation of > or =0.2 mV at 80 msec after the J-point in comparison to the baseline value. The microvascular integrity of the myocardium was evaluated by myocardial contrast echocardiography (MCE) one day after the PCI was performed. Six months later, all of the patients were followed up by echocardiography and the wall motion score index (WMSI) and ejection fraction (EF) were measured.
RESULTS
Significant ST elevation was noted in 47 patients (Group A) after coronary occlusion. There was no significant change in the other 31 patients (Group B). MCE showed microvascular perfusion in 41 patients in group A (87%) and in four patients in group B (13%) (p<0.05). The six-month follow-up echocardiography showed that group A had a lower WMSI (1.20+/-0.18 vs 1.56+/-0.34, p<0.05) and higher EF (57.6+/-7 vs 47+/-11, p<0.05) than group B. The LV end diastolic dimension (LVEDD) in group B was increased compared to group A (p=0.021). The LV end systolic dimension (LVESD) was also increased in group B; however, the LVESD in group A was decreased after six months (p=0.002).
CONCLUSION
IC-ECG during PCI is a simple and useful method for assessing the microvascular integrity of the myocardium and for predicting the long-term improvement of LV function.
MeSH Terms
Figure
Reference
-
1. Rahimtoola SH. The hibernating myocardium. Am Heart J. 1989. 117:211–221.2. Huitink JIM, Visser FC, Bax JJ, Visser CA. Detection of viability after myocardial infarction: available techniques and clinical relevance-a review. Int J Cardiol. 1995. 51:253–266.3. Abaci A, Oguzhan A, Topsakal R, et al. Intracoronary electrocardiogram and angina pectoris during percutaneous coronary interventions as an assessment of myocardial viability: comparison with low-dose dobutamine echocardiography. Catheter Cardiovasc Interv. 2003. 60:469–476.4. Meier B, Killisch JP, Adatte JJ, Casalini P, Rutishauser W. Intrakoronares elektrokardiogram warend transluminaler koronarangioplastie. Schweiz Med Wochenschr. 1985. 115:1590–1593.5. Meier B, Rutishauser W. Coronary pacing during percutaneous transluminal coronary angioplasty. Circulation. 1985. 71:557–561.6. Friedman PL, Shook TL, Kiershenbaum JM, Selwyn A, Ganz P. Value of the intracoronary electrocardiogram to monitor myocardial ischemia during percutaneous transluminal coronary angioplasty. Circulation. 1986. 74:330–339.7. Pande AK, Meier B, Urban P, Moles V, Dorsaz PA, Farve J. Intracoronary electrocardiogram during coronary angioplasty. Am Heart J. 1992. 124:337–341.8. Piessens J, Vrolix M, Sionis D, Glazier JJ, De Geest H, Willems J. The value of the intracoronary electrogram for the early detection of myocardial ischemia during coronary angioplasty. Eur Heart J. 1991. 12:1176–1182.9. Saito S, Watanabe I, Hibiya K, et al. Intracoronary ST-segment alternans during coronary balloon angioplasty. Jpn Heart J. 1998. 39:221–224.10. Yajima J, Saito S, Honye J, Takayama T, Ozawa Y, Kanmatususe K. Intracoronary electrocardiogram for early detection of myocardial viability during coronary angioplasty in acute myocardial infarction. Int J Cardiol. 2001. 79:293–299.11. Ahn JC, Shim WJ, Rha SW, et al. Myocardial reperfusion and long-term change of left ventricular volume after acute anterior wall myocardial infarction. Korean Circ J. 1997. 27:1138–1146.12. Shim WJ. Assessment of myocardial perfusion by myocardial contrast echocardiography. Korean Circ J. 2001. 31:285–289.13. Aggeli C, Theocharis C, Bonou M, Stefanadis C. Contrast echocardiography: a new method for the assessment of myocardial perfusion in coronary artery disease. Hellenic J Cardiol. 2003. 44:400–407.14. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's guidelines and standards committee and the chamber quantification writing group, developed in conjuction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005. 18:1440–1463.15. Porter TR, Xie F, Kricsfeld D, Armbruster RW. Improved myocardial contrast with second harmonic transient ultrasound response imaging in humans using intravenous perfluorocarbon-exposed sonicated dextrose albumin. J Am Coll Cardiol. 1996. 27:1497–1501.16. Min PK, Jung JH, Kang WC, et al. The role of myocardial contrast echocardiography in acute chest pain without ST elevation. Korean Circ J. 2003. 33:284–293.17. Bonow RO, Dilsizian V, Cuocolo A, Bacharach SL. Identification of viable myocardium in patients with chronic coronary artery disease and left ventricular dysfunction: comparison of thallium scintigraphy with reinjection and PET imaging with 18F-fluorodeoxyglucose. Circulation. 1991. 83:26–37.18. Marin-Neto JA, Dilsizian V, Arrighi JA, et al. Thallium reinjection demonstrates viable myocardium in regions with reverse redistribution. Circulation. 1993. 88:1736–1745.19. Pierard LA, De Landsheere CM, Berthe C, Rigo P, Kulbertus HE. Identification of viable myocardium by echocardiography during dobutamine infusion in patients with myocardial infarction after thrombolytic therapy: comparison with positron emission tomography. J Am Coll Cardiol. 1990. 15:1021–1031.20. Watada H, Ito H, Oh H, et al. Dobutamine stress echocardiography predicts reversible dysfunction and quantitates the extent of irreversibly damaged myocardium after reperfusion of anterior myocardial infarction. J Am Coll Cardiol. 1994. 24:624–630.21. Ragosta M, Camarano G, Kaul S, Powers ER, Sarembock IJ, Gimple LW. Microvascular integrity indicates myocellular viability in patients with recent myocardial infarction: new insights using myocardial contrast echocardiography. Circulation. 1994. 89:2562–2569.22. Ito H, Maruyama A, Iwakura K, et al. Clinical implications of no reflow phenomenon: a predictor of complications and left ventricular remodeling in reperfused anterior wall myocardial infarction. Circulation. 1996. 93:223–228.23. Zipes . Braunwald's Heart Disease: a textbook of cardiovascular medicine. 2005. 7th ed. Philadelphia: W.B. Saunders;1216–1218.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- No-Reflow Phoenomenon by Intracoronary Thrombus in Acute Myocardial Infarction
- Intracoronary Thrombolysis and Delayed Percutaneous Coronary Intervention for the Treatment of Large Coronary Thrombi in a Patient with Polycythemia Vera
- A Case of a Successful Percutaneous Coronary Intervention Using Percusurge(r) System in a Massive Intracoronary Thrombi Patient
- Anomalous Origin of the Left Coronary Artery from the Right Sinus of Valsalva, which Presented as Acute Myocardial Infarction
- Intracoronary Stenting in Patients with Acute Myocardial Infarction