Korean J Androl.
2011 Aug;29(2):174-176. 10.5534/kja.2011.29.2.174.
A Case of Xanthogranulomatous Prostatitis Concurrent with a Prostatic Abscess
- Affiliations
-
- 1Department of Urology, Paik Institute, Inje University College of Medicine, Busan, Korea. kweonsikmin@yahoo.com
- 2Department of Pathology, Inje University College of Medicine, Busan, Korea.
- KMID: 2226472
- DOI: http://doi.org/10.5534/kja.2011.29.2.174
Abstract
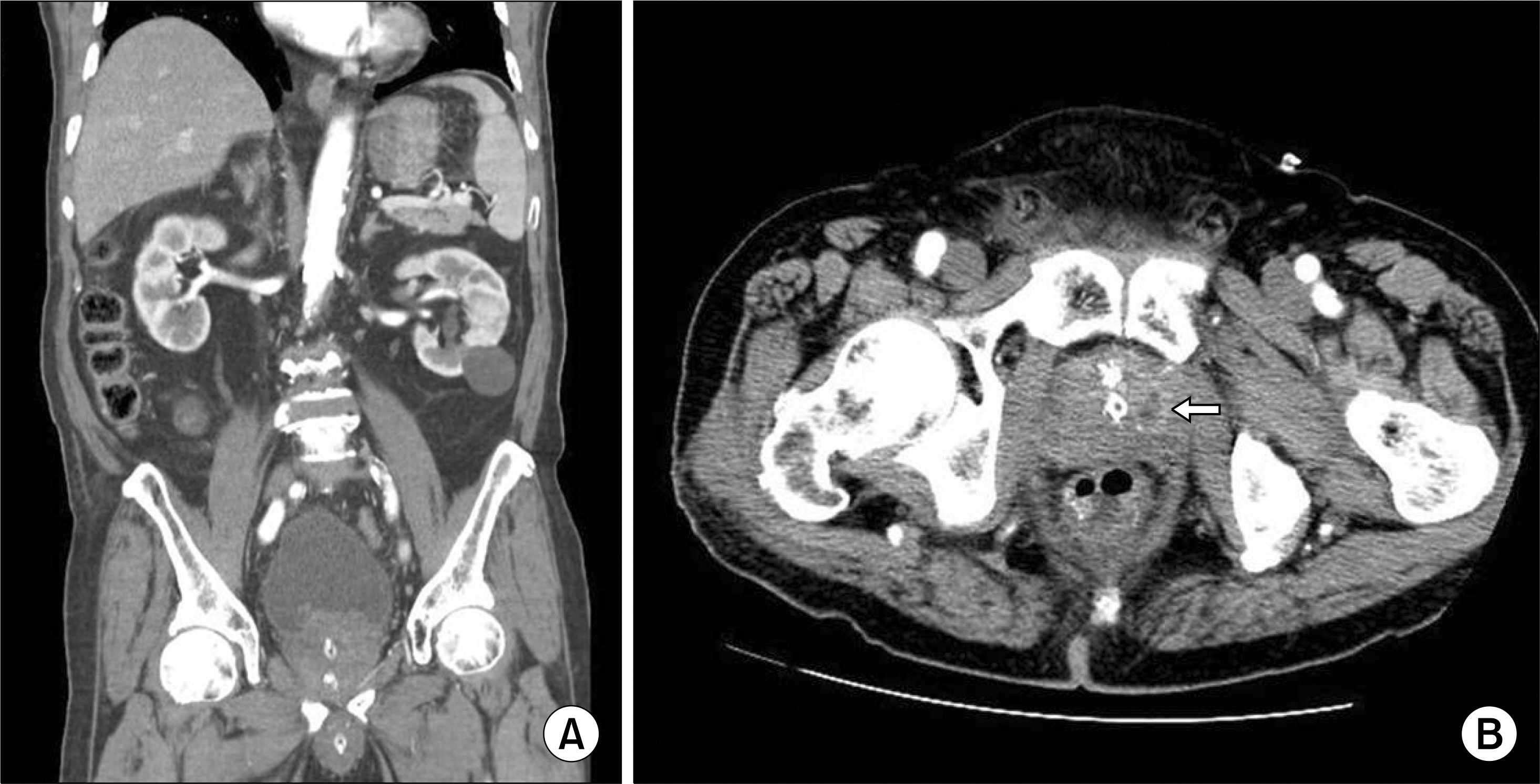
- Xanthogranulomatous prostatitis is a rare inflammatory condition of the prostate. We report a case of xanthogranulomatous prostatitis. An 82-year-old man presented to our emergency department complaining of gross hematuria. A hard, enlarged, non-tender prostate was palpated on digital rectal examination. Urinalysis showed hematuria and pyuria, and the complete blood count (CBC) revealed leukocytosis. The prostate-specific antigen (PSA) level was elevated at 86.8 ng/ml. Computed tomography (CT) showed an enlarged prostate (volume 100 ml) that protruded into the bladder base. In the left lobe of the prostate, a 1.2x1.1-cm abscess was seen. Transurethral resection of the prostate was done. The pathological diagnosis was xanthogranulomatous prostatitis. The natural progression of the disease is unknown because of the paucity of cases and long-term follow-up reports. To evaluate the pathogenesis and long-term features of progression of this disease, more clinical cases should be collected.
Keyword
MeSH Terms
Figure
Reference
-
1). Hayashi N, Wada T, Kiyota H, Ueda M, Oishi Y. Xanthogranulomatous cystitis. Int J Urol. 2003; 10:498–500.
Article2). Epstein JI, Hutchins GM. Granulomatous prostatitis: distinction among allergic, nonspecific, and post-transurethral resection lesions. Hum Pathol. 1984; 15:818–25.
Article3). O'Dea MJ, Hunting DB, Greene LF. Non-specific granulomatous prostatitis. J Urol. 1977; 118:58–60.4). Tanner FH, McDonald JR. Granulomatous prostatits: a histologic study of a group of granulomatous lesions collected from prostate glands. Arch Pathol. 1943; 36:358–70.5). Epstein JI. The prostate and seminal vesicles. Diagnostic surgical pathology. 2nd ed.New York: Raven;1994. p. 1807–48.6). Stillwell TJ, Engen DE, Farrow GM. The clinical spectrum of granulomatous prostatitis: a report of 200 cases. J Urol. 1987; 138:320–3.
Article7). Rafique M, Yaqoob N. Xanthogranulomatous prostatitis: a mimic of carcinoma of prostate. World J Surg Oncol. 2006; 4:30.
Article8). Srigley JR. Benign mimickers of prostatic adenocarcinoma. Mod Pathol. 2004; 17:328–48.
Article9). Miekoś E, Włodarczyk W, Szram S. Xanthogranulomatous prostatitis. Int Urol Nephrol. 1986; 18:433–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Observation of Prostatic Abscess found during Tranaurethral Resection of Prostate
- The Concentrations of Zinc in Expressed Prostatic Secretion of Chronic Prostatitis Patients
- Determination of Immunoglobulin in Prostatic Secretion of Patients with Prostatitis
- 1 Case of Xanthogranulomatous Pyelonephritis
- Emphysematous Prostatic Abscess Due to Klebsiella pneumoniae: Report of a Case And Review of the Literature