Korean Circ J.
2008 Dec;38(12):666-670. 10.4070/kcj.2008.38.12.666.
Changes in Left Ventricular Systolic Function According to Thrombolysis in Myocardial Infarction Frame Count Immediately After Coronary Intervention in Patients With Obstructive Coronary Artery Disease
- Affiliations
-
- 1Department of Cardiovascular Medicine, School of Medicine, Konkuk University, Seoul, Korea. khryu@kuh.ac.kr
- KMID: 2225700
- DOI: http://doi.org/10.4070/kcj.2008.38.12.666
Abstract
- BACKGROUND AND OBJECTIVES
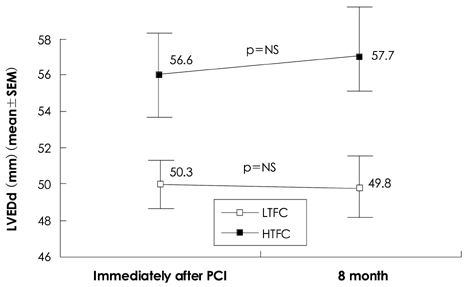
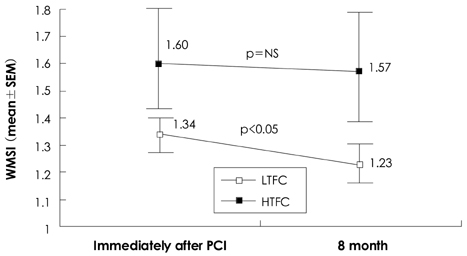
Some reports have suggested that coronary microvascular dysfunction plays a role in the recovery of myocardial function in patients with obstructive coronary artery disease. Thrombolysis in myocardial infarction (TIMI) frame count (TFC) is regarded as a simple, reliable method for evaluating microvascular function. We evaluated microvascular function using TFC immediately after coronary intervention and compared TFC with left ventricular systolic function eight months later. SUBJECTS AND METHODS: We studied 68 patients with obstructive coronary artery disease who underwent coronary intervention. Just after intervention, TFC was calculated with the standard method. Left ventricular systolic function was assessed with left ventricular diastolic dimension (LVEDd), ejection fraction (EF), and wall motion score index (WMSI). Eight months after intervention, we completed follow-up coronary angiography and echocardiography. We defined high TFC (HTFC) as a TFC greater than 18. RESULTS: Ten patients were in the HTFC group, and 58 patients were in the low TFC (LTFC) group. There was no difference between the two groups with regard to baseline cardiovascular characteristics and angiographic findings. Just after intervention, the HTFC group showed significantly higher LVEDd (56.6+/-8.9 mm) and WMSI (1.60+/-0.65) compared to the LTFC group (50.3+/-5.9 mm, p<0.05; 1.34+/-0.29, p<0.05, respectively), but there was no significant difference in EF between the groups (49.3+/-18.6% vs. 56.2+/-14.8%, p>0.05). Eight months after intervention, there was also a significant decrease in the WMSI in the LTFC group (1.23+/-0.25, p<0.05), but not in the HTFC group (1.57+/-0.62, p>0.05). CONCLUSION: Increased TFC immediately after coronary intervention is an important poor prognostic factor related to myocardial systolic function eight months after coronary intervention. Coronary microvascular dysfunction may influence myocardial recovery in the setting of obstructive coronary artery disease.
MeSH Terms
Figure
Reference
-
1. Stone GW, Cox D, Garcia E, et al. Normal flow (TIMI-3) before mechanical reperfusion therapy is an independent determinant of survival in acute myocardial infarction: analysis from the primary angioplasty in myocardial infarction trials. Circulation. 2001. 104:636–641.2. Ndrepepa G, Kastrati A, Schwaiger M, et al. Relationship between residual blood flow in the infarct-related artery and scintigraphic infarct size, myocardial salvage, and functional recovery in patients with acute myocardial infarction. J Nucl Med. 2005. 46:1782–1788.3. Gibson CM, Cannon CP, Murphy SA, et al. Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs. Circulation. 2000. 101:125–130.4. An SG, Oh JH, Park TI, et al. Risk factors for reflow disturbance phenomenon during percutaneous coronary intervention in patients with acute myocardial infarction. Korean J Med. 2008. 74:16–22.5. Park JS, Bae JW, Koo BK, et al. Risk factors of no-reflow phenomenon after primary percutaneous coronary intervention with stent implantation. Korean Circ J. 2004. 34:368–375.6. Gibson CM, Cannon CP, Daley WL, et al. TIMI frame count: a quantitative method of assessing coronary artery flow. Circulation. 1996. 93:879–888.7. Gibson CM, Murphy SA, Rizzo MJ, et al. Relationship between TIMI frame count and clinical outcomes after thrombolytic administration. Circulation. 1999. 99:1945–1950.8. Woo SI, Tahk SJ, Yoon MH, et al. Correlation between thrombolysis in myocardial infarction, the myocardial perfusion grade and the myocardial viability indices after primary percutaneous coronary intervention in ST segment elevation myocardial infarction. Korean Circ J. 2007. 37:581–589.9. Choi SY, Tahk SJ, Yoon MH, et al. Comparison of TIMI myocardial perfusion grade with coronary flow reserve for prediction of recovery of LV function and LV remodeling in acute myocardial infarction. Korean Circ J. 2004. 34:247–257.10. Kim PJ, Jung HO, Koh YS, et al. Comparison of TIMI frame count and TIMI myocardial perfusion grade in assessment of myocardial reperfusion after primary angioplasty for acute myocardial infarction. Korean Circ J. 2003. 33:864–870.11. Ito H, Tomooka T, Sakai N, et al. Lack of myocardial perfusion immediately after successful thrombolysis: a predictor of poor recovery of left ventricular function in anterior myocardial infarction. Circulation. 1992. 85:1699–1705.12. Maes A, van de Werf F, Nuyts J, Bormans G, Desmet W, Mortelmans L. Impaired myocardial tissue perfusion early after successful thrombolysis: impact on myocardial flow, metabolism, and function at late follow-up. Circulation. 1995. 92:2072–2078.13. Hamada S, Nakamura S, Sugiura T, et al. Early detection of the no-reflow phenomenon in reperfused acute myocardial infarction using technetium-99m tetrofosmin imaging. Eur J Nucl Med. 1999. 26:208–214.14. Wakatsuki T, Nakamura M, Tsunoda T, et al. Coronary flow velocity immediately after primary coronary stenting as a predictor of ventricular wall motion recovery in acute myocardial infarction. J Am Coll Cardiol. 2000. 35:1835–1841.15. Gibson CM, Goel M, Cohen DJ, et al. Six-month angiographic and clinical follow-up of patients prospectively randomized to receive either tirofiban or placebo during angioplasty in the RESTORE trial: randomized efficacy study of tirofiban for outcomes and restenosis. J Am Coll Cardiol. 1998. 32:28–34.16. Hamada S, Nishiue T, Nakamura S, et al. TIMI frame count immediately after primary coronary angioplasty as a predictor of functional recovery in patients with TIMI 3 reperfused acute myocardial infarction. J Am Coll Cardiol. 2001. 38:666–671.17. Heyndrickx GR, Amano J, Patrick TA, et al. Effects of coronary artery reperfusion on regional myocardial blood flow and function in conscious baboons. Circulation. 1985. 71:1029–1037.18. Cobb FR, Bache RJ, Rivas F, Greenfield JC Jr. Local effects of acute cellular injury on regional myocardial blood flow. J Clin Invest. 1976. 57:1359–1368.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of Angiographic Outcome by Thrombolysis in Myocardial Infarction(TIMI) Frame Count for Primary Stenting in Patients with Acute Myocardial Infarction
- Simultaneous acute myocardial infarction in two coronary arteries
- 2 Case of Coronary Artery-to-Left Ventricular Fistulae
- Right Ventricular Myocardial Infarction due to Right Coronary Artery Total Occlusion Originating From the Distal Left Circumflex Artery
- Left main artery stenting under percutaneous cardiopulmonary support after right coronary artery ST elevation infarction