Korean Circ J.
2009 Apr;39(4):138-144. 10.4070/kcj.2009.39.4.138.
Association Between Inappropriateness of Left Ventricular Mass and Left Ventricular Diastolic Dysfunction: A Study Using the Tissue Doppler Parameter, E/E'
- Affiliations
-
- 1Cardiology Division, Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea. jhs2003@hanyang.ac.kr
- KMID: 2225688
- DOI: http://doi.org/10.4070/kcj.2009.39.4.138
Abstract
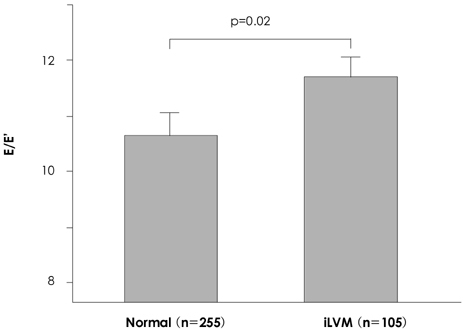
- BACKGROUND AND OBJECTIVES
The structural significance of the inappropriateness of left ventricular mass (iLVM) is known to be an important prognostic factor for cardiovascular events; however, the functional changes associated with iLVM have not been established. This study was performed to determine if diastolic dysfunction is associated with iLVM using a tissue Doppler technique. SUBJECTS AND METHODS: Three hundred sixty consecutive subjects, including 221 hypertension patients from the echocardiography database, were analyzed. Regarding the appropriateness of left ventricular (LV) mass, an observed/predicted ratio of LV mass (OPR) >130% was defined as inappropriate. Echocardiographic parameters, including early diastolic peak velocity (E)/late diastolic peak velocity (A), deceleration time (DT), isovolumetric relaxation time (IVRT), and E/early mitral annulus velocity (E'), were compared between the appropriate LV mass (aLVM) group and the iLVM group. RESULTS: Among transmitral flow parameters, only the E velocity was negatively correlated with the OPR when adjusted for age (adjusted r=-0.107, p=0.04). Based on multiple regression analysis, the OPR (beta=0.163, p=0.003), as well as age (beta=0.286, p=0.0001), systolic blood pressure (beta=0.120, p=0.019), fasting blood glucose (beta=0.098, p=0.042), and male gender (beta=0.157, p=0.002) were independent factors determining E/E'. The cholesterol level was not an independent factor (beta=-0.059, p=0.355). In the iLVM group (n=105), the adjusted E/E' was higher than in the aLVM group (n=255; 11.7+/-3.4 vs. 10.8+/-3.1, p=0.02), while the peak E flow velocity was significantly lower than in the aLVM group (70.9+/-15.1 vs. 75.5+/-17.6, p=0.03). CONCLUSION: Inappropriateness of LV mass is independently associated with increased E/E'. Thus, E/E' may be a useful parameter for the evaluation of diastolic dysfunction.
Keyword
MeSH Terms
Figure
Reference
-
1. Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med. 1990. 322:1561–1566.2. de Simone G, Devereux RB, Kimball TR, et al. Interaction between body size and cardiac workload: influence on left ventricular mass during body growth and adulthood. Hypertension. 1998. 31:1077–1082.3. de Simone G, Verdecchia P, Pede S, Gorini M, Maggioni AP. Prognosis of inappropriate left ventricular mass in hypertension. Hypertension. 2002. 40:470–476.4. Palmieri V, de Simone G, Roman MJ, Schwartz JE, Pickering TG, Devereux RB. Ambulatory blood pressure and metabolic abnormalities in hypertensive subjects with inappropriately high left ventricular mass. Hypertension. 1999. 34:1032–1040.5. de Simone G, Pasanisi F, Contaldo F. Link of nonhemodynamic factors to hemodynamic determinants of left ventricular hypertrophy. Hypertension. 2001. 38:13–18.6. Celentano A, Palmieri V, Esposito ND, et al. Inappropriate left ventricular mass in normotensive and hypertensive patients. Am J Cardiol. 2001. 87:361–363. A107. de Simone G, Kitzman DW, Palmieri V, et al. Association of inappropriate left ventricular mass with systolic and diastolic dysfunction. Am J Hypertens. 2004. 17:828–833.8. World Health Organization. Physical status: the use and interpretation of anthropometry. World Health Organ Tech Rep Ser. 1995. 854:1–452.9. Inoue S, Zimmet P. The Asia-Pacific perspective: redefining obesity and its treatment. Health Communications Australia Pty Limited Sydney. 2000. 2:5–21.10. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001. 285:2486–2497.11. Devereux RB, Alonso DR, Lutas EM, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986. 57:450–458.12. Sohn DW, Choi YJ, Oh BH, Lee MM, Lee YW. Estimation of left ventricular end-diastolic pressure with the difference in pulmonary venous and mitral A durations is limited when mitral E and A waves are overlapped. J Am Soc Echocardiogr. 1999. 12:106–112.13. Lubien E, DeMaria A, Krishnaswamy P, et al. Utility of B-natriuretic peptide in detecting diastolic dysfunction: comparison with Doppler velocity recordings. Circulation. 2002. 105:595–601.14. Shin J, Kim KS, Kim SK, et al. Influences of body size and cardiac workload on the left ventricular mass in healthy Korean adults with normal body weight and blood pressure. Korean Circ J. 2005. 35:335–340.15. Conrady AO, Rudomanov OG, Zaharov DV, et al. Prevalence and determinants of left ventricular hypertrophy and remodelling patterns in hypertensive patients. Blood Press. 2004. 13:101–109.16. Devereux RB, Dahlof B, Gerdts E, et al. Regression of hypertensive left ventricular hypertrophy by losartan compared with atenolol. Circulation. 2004. 110:1456–1462.17. Racette SB, Evans EM, Weiss EP, Hagberg JM, Holloszy JO. Abdominal adiposity is a stronger predictor of insulin resistance than fitness among 50-95 year olds. Diabetes Care. 2006. 29:673–678.18. Price GM, Uauy R, Breeze E, Bulpitt CJ, Fletcher AE. Weight, shape, and mortality risk in older persons: elevated waist-hip ratio, not high body mass index, is associated with a greater risk of death. Am J Clin Nutr. 2006. 84:449–460.19. Ix JH, Shlipak MG, Chertow GM, Ali S, Schiller NB, Whooley MA. Cystatin C, left ventricular hypertrophy, and diastolic dysfunction. J Card Fail. 2006. 12:601–607.20. Ferrara LA, Vaccaro O, Cardoni O, Laurenzi M, Mancini M, Zanchetti A. Indexation criteria of ventricular mass and predictive role of blood pressure and body composition. Am J Hypertens. 2005. 18:1282–1287.21. De Sutter J, De Backer J, van de Veire N, Velghe A, De Buyzere M, Gillebert TC. Effects of age, gender, and left ventricular mass on septal mitral annulus velocity (E') and the ratio of transmitral early peak velocity to E' (E/E'). Am J Cardiol. 2005. 95:1020–1023.22. Rovner A, de las Fuentes L, Waggoner AD, Memon N, Chohan R, Dávila-Román VG. Characterization of left ventricular diastolic function in hypertension by use of Doppler tissue imaging and color M-mode techniques. J Am Soc Echocardiogr. 2006. 19:872–879.23. Ahn HS, Kim SJ, Kim MK, et al. The difference of left ventricular hypertrophy and diastolic function between prehypertensives and normotensives. Korean Circ J. 2006. 36:437–442.24. Cho KI, Park JH, Lee CK, et al. Isolated and combined influences of diabetes and hypertension on the myocardial function and geometry. Korean Circ J. 2006. 36:411–417.25. Kim MH, Kim MK, Choi BY, Shin YJ. Prevalence of the metabolic syndrome and its association with cardiovascular diseases in Korea. J Korean Med Sci. 2004. 19:195–201.26. Lee SY, Park HS, Kim DJ, et al. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract. 2007. 75:72–80.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Left ventricular hypertrophy and diastolic function in children and adolescents with essential hypertension
- The Role of Doppler Time Index for Evaluation of Left Ventricular Diastolic Function by Patterns of Left Ventricular Hypertrophy in Hypertensive Patients
- A Study for Diastolic Functions in Patients with Early Acute Myocardial Infarction
- Left Ventricular Diastolic Functions by M-Mode Echocardiogram in Essential Hypertensive Patients
- Assessment of Diastolic Function Using Mitral Annulus Velocity by Doppler Tissue Velocity in the Patients with Left Ventricular Hypertrophy