Korean Circ J.
2009 Sep;39(9):378-381. 10.4070/kcj.2009.39.9.378.
The Best Predictor for Right Ventricular Dysfunction in Acute Pulmonary Embolism: Comparison Between Electrocardiography and Biomarkers
- Affiliations
-
- 1Department of Cardiology, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. dgpark@hallym.or.kr
- 2Department of Cardiology, Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea.
- KMID: 2225674
- DOI: http://doi.org/10.4070/kcj.2009.39.9.378
Abstract
- BACKGROUND AND OBJECTIVES
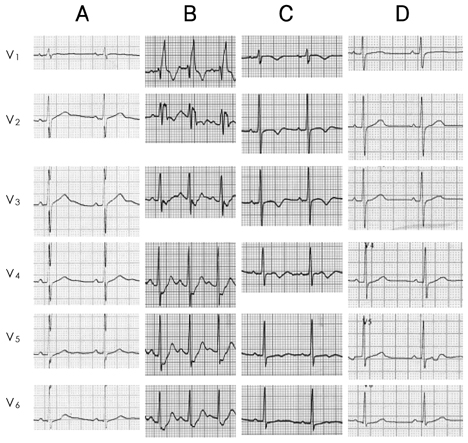
Right ventricular (RV) dysfunction is associated with a poor prognosis in patients with an acute pulmonary embolism (APE). We studied the role of electrocardiography and biomarkers for early detection and recovery of right ventricular dysfunction (RVD) in APE. SUBJECTS AND METHODS: The medical records of 48 consecutive patients diagnosed with APE using CT-angiography, at the Kangdong Sacred Heart Hospital, between January 2004 and February 2008 were reviewed retrospectively. RVD was assessed by serial echocardiography (ECG). Patients with one of the following were considered to have RVD: 1) RV dilatation (enddiastolic diameter >30 mm in the parasternal long axis view), 2) RV free wall hypokinesia, and 3) paradoxical septal systolic motion. We compared the electrocardiographic findings and the biomarkers for the early detection of RVD. RESULTS: The electrocardiographic findings showed T-wave inversion (TWI) in leads V1 to V3 with a sensitivity of 75% and a specificity of 95%, and a diagnostic accuracy of 80% for the detection of RVD, with positive and negative predictive values of 95.5% and 73.1%, respectively; these results were better than the biomarkers such as cardiac enzymes or B-type natriuretic peptide (BNP) for the early detection of RVD. TWIs persisted throughout the period of RVD, in contrast to a transient S1Q3T3 pattern detected during the acute phase only. CONCLUSION: TWIs in leads V1 to V3 had the greatest sensitivity and diagnostic accuracy for early detection of RVD, and normalization of the TWIs was associated with recovery of RVD in APE.
MeSH Terms
Figure
Reference
-
1. Stein PD, Beemath A, Matta F, et al. Enlarged right ventricle without shock in acute pulmonary embolism: prognosis. Am J Med. 2008. 121:34–42.2. Kreit JW. The impact of right ventricular dysfunction on the prognosis and therapy of normotensive patients with pulmonary embolism. Chest. 2004. 125:1539–1545.3. Wolfe MW, Lee RT, Feldstein ML, Parker JA, Come PC, Goldhaber SZ. Prognostic significance of right ventricular hypokinesis and perfusion lung scan defects in pulmonary embolism. Am Heart J. 1994. 127:1371–1375.4. Lualdi JC, Goldhaber SZ. Right ventricular dysfunction after acute pulmonary embolism: pathophysiologic factors, detection, and therapeutic implications. Am Heart J. 1995. 130:1276–1282.5. Kasper W, Konstantinides S, Geibel A, Tiede N, Krause T, Just H. Prognostic significance of right ventricular afterload stress detected by echocardiography in patients with clinically suspected pulmonary embolism. Heart. 1997. 77:346–349.6. Aksay E, Yanturali S, Kiyan S. Can elevated troponin I levels predict complicated clinical course and inhospital mortality in patients with acute pulmonary embolism? Am J Emerg Med. 2007. 25:138–143.7. Amorim S, Dias P, Rodrigues RA, et al. Troponin I as a marker of right ventricular dysfunction and severity of pulmonary embolism. Rev Port Cardiol. 2006. 25:181–186.8. Pieralli F, Olivotto I, Vanni S, et al. Usefulness of bedside testing for brain natriuretic peptide to identify right ventricular dysfunction and outcome in normotensive patients with acute pulmonary embolism. Am J Cardiol. 2006. 97:1386–1390.9. Punukollu G, Khan IA, Gowda RM, Lakhanpal G, Vasavada BC, Sacchi TJ. Cardiac troponin I release in acute pulmonary embolism in relation to the duration of symptoms. Int J Cardiol. 2005. 99:207–211.10. Kruger S, Graf J, Merx MW, et al. Brain natriuretic peptide predicts right heart failure in patients with acute pulmonary embolism. Am Heart J. 2004. 147:60–65.11. La Vecchia L, Ottani F, Favero L, et al. Increased cardiac troponin I on admission predicts in-hospital mortality in acute pulmonary embolism. Heart. 2004. 90:633–637.12. Pruszczyk P, Bochowicz A, Torbicki A, et al. Cardiac troponin T monitoring identifies high-risk group of normotensive patients with acute pulmonary embolism. Chest. 2003. 123:1947–1952.13. Kosuge M, Kimura K, Ishikawa T, et al. Prognostic significance of inverted T waves in patients with acute pulmonary embolism. Circ J. 2006. 70:750–755.14. Geibel A, Zehender M, Kasper W, Olschewski M, Klima C, Konstantinides SV. Prognostic value of the ECG on admission in patients with acute major pulmonary embolism. Eur Respir J. 2005. 25:843–848.15. Punukollu G, Gowda RM, Vasavada BC, Khan IA. Role of electrocardiography in identifying right ventricular dysfunction in acute pulmonary embolism. Am J Cardiol. 2005. 96:450–452.16. Sarin S, Elmi F, Nassef L. Inverted T waves on electrocardiogram: myocardial ischemia versus pulmonary embolism. J Electrocardiol. 2005. 38:361–363.17. Kwak MH, Oh J, Jeong JO, et al. Role of echocardiography as a screening test in patients with suspected pulmonary embolism. Korean Circ J. 2001. 31:500–506.18. Yoon NS, Cho JG, Park HW, et al. Usefulness of the 12-lead electrocardiography in the diagnosis and evaluation of severity of pulmonary thromboembolism. Korean Circ J. 2005. 35:389–395.19. Yoshinaga T, Ikeda S, Nishimura E, et al. Serial changes in negative T wave on electrocardiogram in acute pulmonary thromboembolism. Int J Cardiol. 1999. 72:65–72.20. Zhu L, Yang YH, Wu YF, Zhai ZG, Wang C. Value of transthoracic echocardiography combined with cardiac troponin I in risk stratification in acute pulmonary thromboembolism. Chin Med J. 2007. 120:17–21.21. Lui CY. Acute pulmonary embolism as the cause of global T wave inversion and QT prolongation: a case report. J Electrocardiol. 1993. 26:91–95.22. Grifoni S, Vanni S, Magazzini S, et al. Association of persistent right ventricular dysfunction at hospital discharge after acute pulmonary embolism with recurrent thromboembolic events. Arch Intern Med. 2006. 166:2151–2156.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Consecutive Right and Left Ventricular Dysfunction
- Normalization of Negative T-Wave on Electrocardiography and Right Ventricular Dysfunction in Patients with an Acute Pulmonary Embolism
- Diagnosis of Right Ventricular Dysfunction in Acute Pulmonary Embolism with N-terminal Probrain Natriuretic Peptide (NT-proBNP)
- Marked QT prolongation and T inversion in a patient with acute pulmonary thromboembolism
- Are the Cardiac Biomarkers in the Emergency Room Sufficient to Predict Adverse Events in Acute Pulmonary Embolism?