Korean Circ J.
2011 Feb;41(2):91-96. 10.4070/kcj.2011.41.2.91.
Evaluation of Local Flow Conditions in Jailed Side Branch Lesions Using Computational Fluid Dynamics
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. bkkoo@snu.ac.kr
- 2Cardiovascular Center, Seoul National University Hospital, Seoul, Korea.
- 3Department of Emergency Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 4Institute of Medical and Biological Engineering, Medical Research Center, Seoul National University, Seoul, Korea.
- KMID: 2225141
- DOI: http://doi.org/10.4070/kcj.2011.41.2.91
Abstract
- BACKGROUND AND OBJECTIVES
Lesions of vascular bifurcation and their treatment outcomes have been evaluated by anatomical and physiological methods, such as intravascular ultrasound and fractional flow reserve (FFR). However, local changes in flow dynamics in lesions of bifurcation have not been well evaluated. This study aimed at evaluating changes in the local flow patterns of bifurcation lesions.
MATERIALS AND METHODS
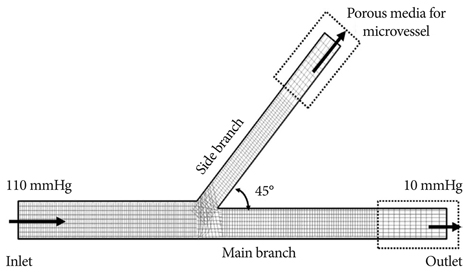
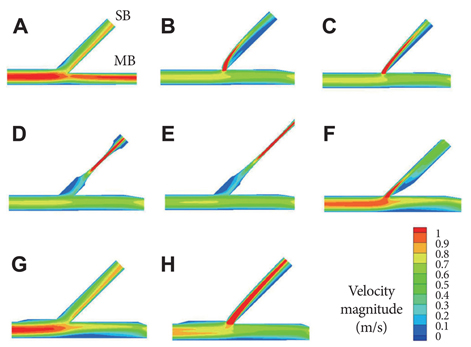
Eight (n=8) representative simulation-models were constructed: 1 normal bifurcation, 5 main-branch (MB) stenting models with various side-branch (SB) stenoses (ostial or non-ostial 75% diameter stenosis with 1- or 2-cm lesion lengths, ostial 75% diameter stenosis caused by carina shift), and 2 post-kissing models (no or 50% SB residual stenosis). Pressure, velocity, and wall shear stress (WSS) profiles around the bifurcation sites were investigated using computational fluid dynamics.
RESULTS
Post-stenting models revealed significant pressure drop in the SB (FFR<0.75), excluding the carina shift model (FFR=0.89). In the post-kissing models, there was no significant pressure drop. All post-stenting models revealed eccentric low velocity flow patterns and areas of low WSS, primarily in the lateral wall on distal MB. Post-kissing angioplasty improved pressure drop in the SB but resulted in alteration of flow distribution in the MB. In the carina shift model, kissing ballooning resulted in deteriorated local flow conditions due to increased area of low velocity and WSS.
CONCLUSION
This study suggests that the most commonly used bifurcation intervention strategy may cause local flow disturbances, which may partially explain high restenosis and event rates in patients with bifurcation lesions.
Keyword
MeSH Terms
Figure
Reference
-
1. Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics-2010 update: a report from the American Heart Association. Circulation. 2010. 121:e46–e215.2. Sharma SK, Mares AM, Kini AS. Coronary bifurcation lesions. Minerva Cardioangiol. 2009. 57:667–682.3. Ferenc M, Gick M, Kienzle RP, et al. Randomized trial on routine vs. provisional T-stenting in the treatment of de novo coronary bifurcation lesions. Eur Heart J. 2008. 29:2859–2867.4. Colombo A, Bramucci E, Sacca S, et al. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus-Eluting Stents) Study. Circulation. 2009. 119:71–78.5. Colombo A, Moses JW, Morice MC, et al. Randomized study to evaluate sirolimus-eluting stents implanted at coronary bifurcation lesions. Circulation. 2004. 109:1244–1249.6. Koo BK, Fitzgerald PJ. Novel coronary stent platforms. Korean Circ J. 2008. 38:393–397.7. Chatzizisis YS, Coskun AU, Jonas M, Edelman ER, Feldman CL, Stone PH. Role of endothelial shear stress in the natural history of coronary atherosclerosis and vascular remodeling: molecular, cellular, and vascular behavior. J Am Coll Cardiol. 2007. 49:2379–2393.8. Malek AM, Alper SL, Izumo S. Hemodynamic shear stress and its role in atherosclerosis. JAMA. 1999. 282:2035–2042.9. Stone PH, Coskun AU, Kinlay S, et al. Effect of endothelial shear stress on the progression of coronary artery disease, vascular remodeling, and instent restenosis in humans: in vivo 6-month follow-up study. Circulation. 2003. 108:438–444.10. LaDisa JF Jr, Olson LE, Molthen RC, et al. Alterations in wall shear stress predict sites of neointimal hyperplasia after stent implantation in rabbit iliac arteries. Am J Physiol Heart Circ Physiol. 2005. 288:H2465–H2475.11. Murata T, Hiro T, Fujii T, et al. Impact of the cross-sectional geometry of the post-deployment coronary stent on in-stent neointimal hyperplasia: an intravascular ultrasound study. Circ J. 2002. 66:489–493.12. Finet G, Gilard M, Perrenot B, et al. Fractal geometry of arterial coronary bifurcations: a quantitative coronary angiography and intravascular ultrasound analysis. EuroIntervention. 2008. 3:490–498.13. Pflederer T, Ludwig J, Ropers D, Daniel WG, Achenbach S. Measurement of coronary artery bifurcation angles by multidetector computed tomography. Invest Radiol. 2006. 41:793–798.14. Wang JC, Normand SL, Mauri L, Kuntz RE. Coronary artery spatial distribution of acute myocardial infarction occlusions. Circulation. 2004. 110:278–284.15. Yull Park J, Young Park C, Mo Hwang C, Sun K, Goo Min B. Pseudo-organ boundary conditions applied to a computational fluid dynamics model of the human aorta. Comput Biol Med. 2007. 37:1063–1072.16. Koo BK, Waseda K, Kang HJ, et al. Anatomic and functional evaluation of bifurcation lesions undergoing percutaneous coronary intervention. Circ Cardiovasc Interv. 2010. 3:113–119.17. Pijls NH, De Bruyne B, Peels K, et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med. 1996. 334:1703–1708.18. Pijls NH. Optimum guidance of complex PCI by coronary pressure measurement. Heart. 2004. 90:1085–1093.19. Suh JW, Koo BK, Jo SH, et al. Optimal dosage and method of administration of adenosine for measuring the coronary flow reserve and the fractional flow reserve in Koreans. Korean Circ J. 2006. 36:300–307.20. Park KH, Koo BK, Shu JH, et al. Assessment of intermediate coronary stenosis in Koreans using the fractional flow reserve. Korean Circ J. 2008. 38:468–474.21. Ikeno F, Kim YH, Luna J, et al. Acute and long-term outcomes of the novel side access (SLK-View) stent for bifurcation coronary lesions: a multicenter nonrandomized feasibility study. Catheter Cardiovasc Interv. 2006. 67:198–206.22. Lefevre T, Ormiston J, Guagliumi G, et al. The Frontier stent registry: safety and feasibility of a novel dedicated stent for the treatment of bifurcation coronary artery lesions. J Am Coll Cardiol. 2005. 46:592–598.23. Ormiston J, Webster M, El-Jack S, McNab D, Plaumann SS. The AST petal dedicated bifurcation stent: first-in-human experience. Catheter Cardiovasc Interv. 2007. 70:335–340.24. Sharma SK, Kini AS. Coronary bifurcation lesions. Cardiol Clin. 2006. 24:233–246.25. Louvard Y, Lefevre T, Morice MC. Percutaneous coronary intervention for bifurcation coronary disease. Heart. 2004. 90:713–722.26. Melikian N, Di Mario C. Treatment of bifurcation coronary lesions: a review of current techniques and outcome. J Interv Cardiol. 2003. 16:507–513.27. Steigen TK, Maeng M, Wiseth R, et al. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation. 2006. 114:1955–1961.28. Williams AR, Koo BK, Gundert TJ, Fitzgerald PJ, LaDisa JF Jr. Local hemodynamic changes caused by main branch stent implantation and subsequent virtual side branch balloon angioplasty in a representative coronary bifurcation. J Appl Physiol. 2010. 109:532–540.29. Niemela M, Kervinen K, Erglis A, et al. Randomized comparison of final kissing balloon dilatation versus no final kissing balloon dilatation in patients with coronary bifurcation lesions treated with main vessel stenting: the Nordic-Baltic Bifurcation Study III. Circulation. 2011. 123:79–86.30. Gwon HC, Choi SH, Song YB, et al. Long-term clinical results and predictors of adverse outcomes after drug-eluting stent implantation for bifurcation lesions in a real-world practice: the COBIS (Coronary Bifurcation Stenting) registry. Circ J. 2010. 74:2322–2328.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Considerations of Blood Properties, Outlet Boundary Conditions and Energy Loss Approaches in Computational Fluid Dynamics Modeling
- Consecutive Jailed- and Kissing-Corsair Technique: Side Branch Protection and Dilation during Stent Implantation
- Computational Fluid Dynamics Modeling in Aortic Diseases
- Computational Fluid Dynamics of Intracranial Artery Using 3-Dimensional Angiography: Potentials and Technical Considerations
- Computational Fluid Dynamics in Three Dimensional Angiography: Preliminary Hemodynamic Results of Various Proximal Geometry