Korean Circ J.
2011 Feb;41(2):68-75. 10.4070/kcj.2011.41.2.68.
Effect of Aspiration Thrombectomy on Microvascular Dysfunction in ST-Segment Elevation Myocardial Infarction With an Elevated Neutrophil Count
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. byungokim@paik.ac.kr
- KMID: 2225138
- DOI: http://doi.org/10.4070/kcj.2011.41.2.68
Abstract
- BACKGROUND AND OBJECTIVES
Aspiration thrombectomy (AT) during primary percutaneous coronary intervention (PCI) is an effective adjunctive therapy for ST-segment elevation myocardial infarction (STEMI). An elevated neutrophil count in STEMI is associated with microvascular dysfunction and adverse outcomes. We evaluated whether AT can improve microvascular dysfunction in patients with STEMI and an elevated neutrophil count.
SUBJECTS AND METHODS
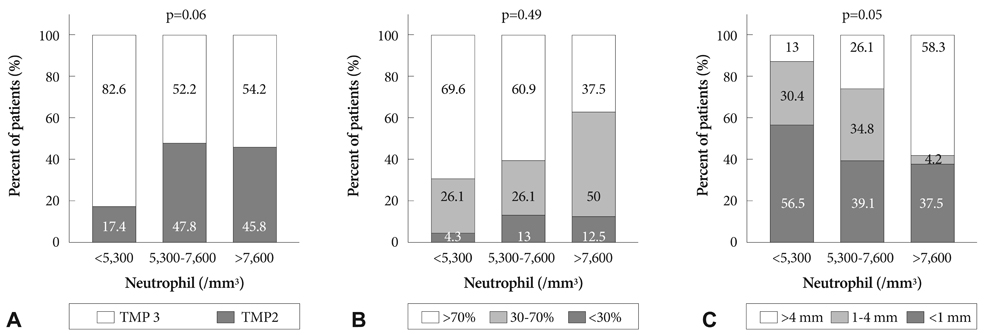
Seventy patients with STEMI undergoing primary PCI from August 2007 to February 2009 in our institution were classified by tertiles of neutrophil count on admission (<5,300/mm3, 5,300-7,600/mm3, and >7,600/mm3). The angiographic outcome was post-procedural thrombolysis in myocardial infarction (TIMI) flow grade. Microvascular dysfunction was assessed by TIMI myocardial perfusion (TMP) grade and ST-segment resolution on electrocardiography 90 minutes after PCI. The clinical outcome was major adverse cardiac event (MACE), defined as cardiac death, re-infarction, and target lesion revascularization at 9 months.
RESULTS
There were no significant differences in the clinical characteristics and pre- and post-procedural TIMI flow grades between the neutrophil tertiles. As the neutrophil count increased, a lower tendency toward TMP grade 3 (83% vs. 52% vs. 54%, p=0.06) and more persistent residual ST-segment elevation (>4 mm: 13% vs. 26% vs. 58%, p=0.005) was observed. The 9-month MACE rate was similar between the groups. On subgroup analysis of AT patients (n=52) classified by neutrophil tertiles, the same tendency toward less frequent TMP grade 3 (77% vs. 56% vs. 47%, p=0.06) and persistent residual ST-segment elevation (>4 mm: 12% vs. 28% vs. 53%, p=0.05) was observed as neutrophil count increased.
CONCLUSION
A higher neutrophil count at presentation in STEMI is associated with more severe microvascular dysfunction after primary PCI, which is not improved with AT.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Efficacy of Combination Treatment with Intracoronary Abciximab and Aspiration Thrombectomy on Myocardial Perfusion in Patients with ST-Segment Elevation Myocardial Infarction Undergoing Primary Coronary Stenting
Sung Gyun Ahn, Seung-Hwan Lee, Ji Hyun Lee, Jun-Won Lee, Young Jin Youn, Min-Soo Ahn, Jang-Young Kim, Byung-Su Yoo, Junghan Yoon, Kyung-Hoon Choe, Seung-Jea Tahk
Yonsei Med J. 2014;55(3):606-616. doi: 10.3349/ymj.2014.55.3.606.
Reference
-
1. Arakawa K, Yasuda S, Hao H, et al. Significant association between neutrophil aggregation in aspirated thrombus and myocardial damage in patients with ST-segment elevation acute myocardial infarction. Circ J. 2009. 73:139–144.2. Kang WC, Ahn TH, Han SH, et al. Efficacy of thrombosuction using the export aspiration catheter before primay percutaneous coronary intervention in acute myocardial infarction. Korean Circ J. 2005. 35:172–179.3. Koh YY, Kim WG, Hwang HK. Aspiration thromboembolectomy in the management of acute coronary occlusion during percutaneous transluminal coronary angiography. Korean Circ J. 1998. 28:1905–1909.4. Huang G, Zhong XN, Zhong B, et al. Significance of white blood cell count and its subtypes in patients with acute coronary syndrome. Eur J Clin Invest. 2009. 39:348–358.5. Chia S, Nagurney JT, Brown DF, et al. Association of leukocyte and neutrophil counts with infarct size, left ventricular function and outcomes after percutaneous coronary intervention for ST-elevation myocardial infarction. Am J Cardiol. 2009. 103:333–337.6. Tamhane UU, Aneja S, Montgomery D, Rogers EK, Eagle KA, Gurm HS. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am J Cardiol. 2008. 102:653–657.7. Turner SJ, Ketch TR, Gandhi SK, Sane DC. Routine hematologic clinical test and prognostic markers in patients with acute coronary syndrome. Am Heart J. 2008. 155:806–816.8. Sezer M, Okcular I, Goren T, et al. Association of haematologic indices with the degree of microcvascular injury in patients with acute anterior wall myocardial infarction treated with primary percutaneous coronary intervention. Heart. 2007. 93:313–318.9. Takahashi T, Hiasa Y, Ohara Y, et al. Relation between neutrophil counts on admission, microvascular injury, and left ventricular functional recovery in patients with an anterior wall first acute myocardial infarction treated with primary coronary angioplasty. Am J Cardiol. 2007. 100:35–40.10. Mariani M, Fetiveau R, Rossetti E, et al. Significance of total and differential leukocyte count in patients with acute myocardial infarction treated with primary coronary angioplasty. Eur Heart J. 2006. 27:2511–2515.11. van 't Hof AW, Liem A, Suryapranata H, Hoorntje JC, de Boer MJ, Zijlstra F. Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction: myocardial blush grade. Circulation. 1998. 97:2302–2306.12. Svilaas T, Vlaar PJ, van der Hosr IC, et al. Thrombus aspiration during primary percutaneous coronary intervention. N Engl J Med. 2008. 358:557–567.13. Javaid A, Siddiqi NH, Steinberg DH, et al. Adjunct thrombus aspiration reduces mortality in patients undergoing percutaneous coronary intervention for ST-elevation myocardial infarction with high-risk angiographic characteristics. Am J Cardiol. 2008. 101:452–456.14. Kirtane AJ, Bui A, Murphs SA, Barron HV, Gibson DM. Association of peripheral neutrophilia with adverse angiographic outcome in ST-elevation myocardial infarction. Am J Cardiol. 2004. 93:532–536.15. Mehta JL, Nichols WW, Mehta P. Neutrophils as potential participants in acute myocardial ischemia: relevance to reperfusion. J Am Coll Cardiol. 1988. 11:1309–1316.16. Nichols WW, Metha HL, Donnelly WH, Lawson D, Thompson L, ter Riet M. Reduction in coronary vasodilator reserve following coronary occlusion and reperfusion in anesthetized dog: role of endothelium derived relaxing factor, myocardial neutrophil infiltration and prostaglandins. J Mol Cell Cardiol. 1988. 20:943–954.17. Kloner RA, Giacomelli F, Alker KJ, Hale SL, Matthews R, Bellows S. Influx of neutrophils in the walls of large epicardail coronary arteries in response to ischemia/perfusion. Circulation. 1991. 84:1758–1772.18. Miyao Y, Miyazaki S, Goto Y, et al. Role of cytokines and adhesion molecules in ischemia and reperfusion in patients with acute myocardial infarction. Jpn Circ J. 1999. 63:362–366.19. Merlini PA, Cugno M, Rossi ML, et al. Activation of the contact system and inflammation after thrombolytic therapy in patients with acute myocardial infarction. Am J Cardiol. 2004. 93:822–825.20. Sabatine MS, Morrow DA, Cannon CP, et al. Relationship between baseline white blood cell count and degree of coronary artery disease and mortality in patients with acute coronary syndromes: A TACTICS-TIMI 18 substudy. J Am Coll Cardiol. 2002. 40:1761–1768.21. Shin SH, Oh DJ, Lim HE, et al. The source of inflammatory response and platelet activation in patients with acute myocardial infarction. Korean Circ J. 2005. 35:155–162.22. Kim KY, Hae JH. The clinical usefulness of decreased mean platelet component concentration in patients with acute coronay syndrome. Korean Circ J. 2005. 35:240–246.23. Han J, Youn TJ, Hong ES, et al. The relationship between initial leukocyte count and the extent of myocardial injury in patients with acute myocardial infarction who received reperfusion therapy. Korean Circ J. 2004. 34:735–742.24. Lee JH, Kim HS, Kwon YS, et al. The prognostic value of mean platelet volume in acute myocardial infarction. Korean Circ J. 2003. 33:878–883.25. Mongeon FP, Bélisle P, Joseph L, Eisenberg MJ, Rinfret S. Adjunctive thrombectomy for acute myocardial infarction: a bayesian meta-analysis. Circ Cardiovasc Interv. 2010. 3:6–16.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of ST-Segment Elevation in a Patient with Subarachnoid Hemorrhage
- ST segment
- Acute Myocardial Infarction by Right Coronary Artery Occlusion Presenting as Precordial ST Elevation on Electrocardiography
- Differences in Clinical Outcomes Between Patients With ST-Elevation Versus Non-ST-Elevation Acute Myocardial Infarction in Korea
- Erratum: Etiologies and Predictors of False-Positive Diagnosis of ST-Segment Elevation Myocardial Infarction