Korean Circ J.
2013 May;43(5):309-315. 10.4070/kcj.2013.43.5.309.
Prediction of Fractional Flow Reserve without Hyperemic Induction Based on Resting Baseline Pd/Pa
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine and Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea. junehongk@gmail.
- 2Department of Mechanical Engineering, Dong-A University, Busan, Korea.
- KMID: 2224923
- DOI: http://doi.org/10.4070/kcj.2013.43.5.309
Abstract
- BACKGROUND AND OBJECTIVES
The purposes of this study are 1) to investigate the relationship between resting baseline Pd/Pa, determined by the ratio of the pressures proximal (Pa) and distal (Pd) to the target lesion before, inducing hyperemia and fractional flow reserve (FFR) and 2) to identify a resting baseline Pd/Pa range that might reliably preclude the need for hyperemic induction.
SUBJECTS AND METHODS
A total of 622 pressure wire data sets obtained from intermediate stenotic lesions were analyzed.
RESULTS
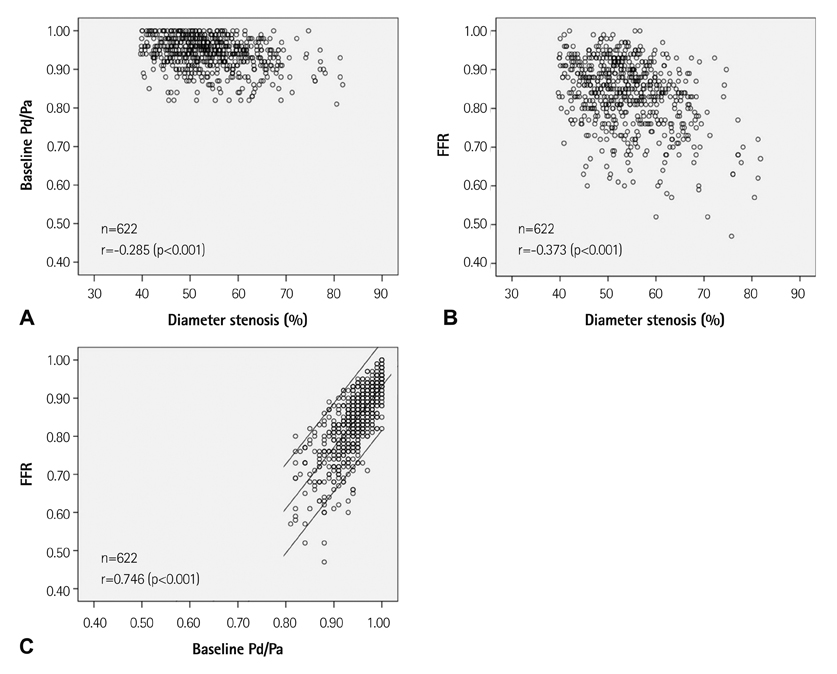
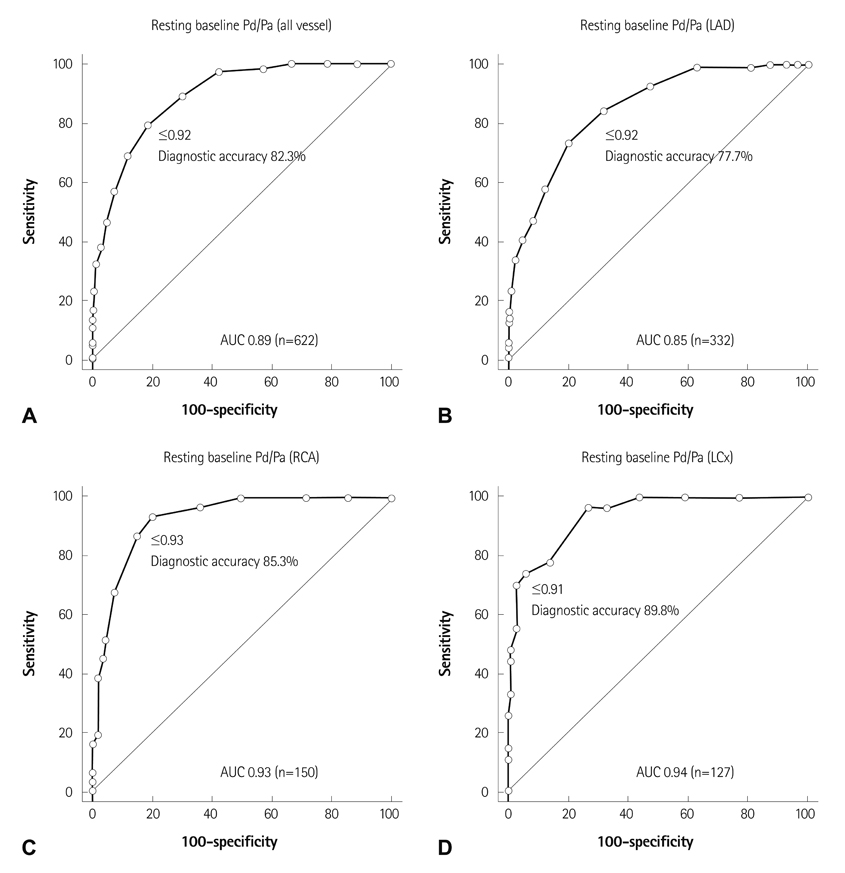
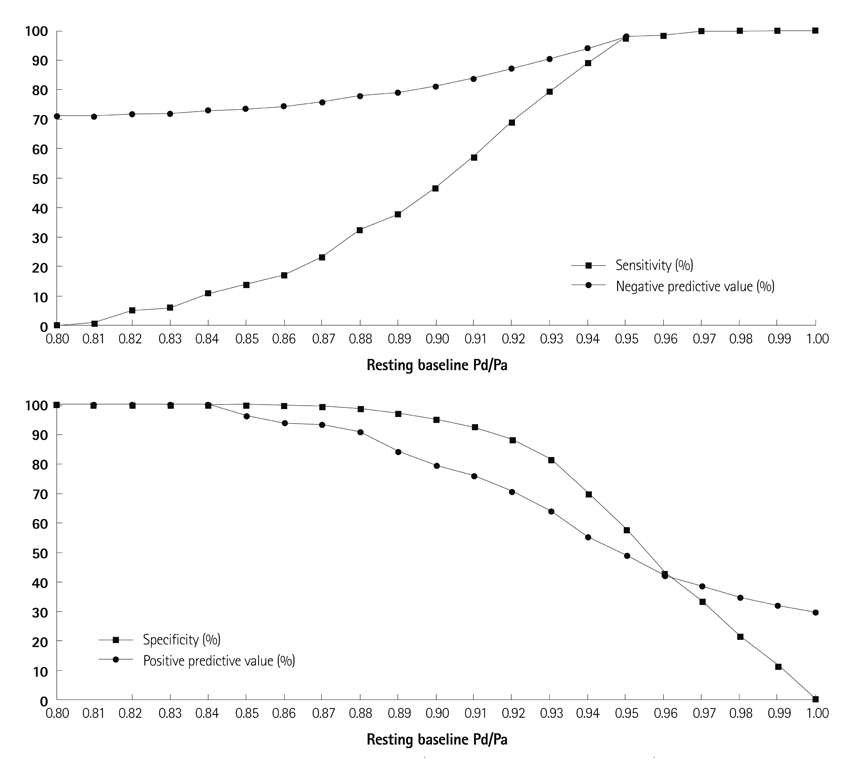
There was a good linear relationship between resting baseline Pd/Pa and FFR (r=0.746, p<0.001). Receiver-operating characteristic curves of the resting baseline Pd/Pa with FFR < or =0.80 as the reference variable showed an area under the curve of 0.89 (95% confidence intervals 0.863-0.914, p<0.001) with a diagnostic accuracy of 82.3% when the resting baseline Pd/Pa was < or =0.92. These results showed that certain cutoff values can reliably predict FFR, whether positive or negative. The resting baseline Pd/Pa >0.95 (n=257, 41.3%) had a negative predictive value (NPV) of 98.1% and a sensitivity of 97.3%. the resting baseline Pd/Pa < or =0.88 (n=65, 10.5%) had a positive predictive value (PPV) of 96.2% and a specificity of 99.8%. These were consistent regardless of coronary vessel, lesion location, lesion length, or degree of stenosis.
CONCLUSION
In intermediate lesions, the resting baseline Pd/Pa was linearly related to FFR. A certain range of the resting baseline Pd/Pa values had an excellent NPV with high sensitivity or excellent PPV with high specificity for determining the lesion significance.
MeSH Terms
Figure
Reference
-
1. Tobis J, Azarbal B, Slavin L. Assessment of intermediate severity coronary lesions in the catheterization laboratory. J Am Coll Cardiol. 2007; 49:839–848.2. Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2011; 124:e574–e651.3. Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). European Association for Percutaneous Cardiovascular Interventions (EAPCI). Wijns W, et al. Guidelines on myocardial revascularization. Eur Heart J. 2010; 31:2501–2555.4. Pijls NH, van Son JA, Kirkeeide RL, De Bruyne B, Gould KL. Experimental basis of determining maximum coronary, myocardial, and collateral blood flow by pressure measurements for assessing functional stenosis severity before and after percutaneous transluminal coronary angioplasty. Circulation. 1993; 87:1354–1367.5. Kim JH, Park JH, Choo K, et al. Pressure-wire based assessment of microvascular resistance using calibrated upstream balloon obstruction: a predictor of myocardial viability. Catheter Cardiovasc Interv. 2012; 80:581–589.6. Sen S, Escaned J, Malik IS, et al. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave-intensity analysis: results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) study. J Am Coll Cardiol. 2012; 59:1392–1402.7. Berry C, van't Veer M, Witt N, et al. VERIFY (VERification of Instantaneous Wave-Free Ratio and Fractional Flow Reserve for the Assessment of Coronary Artery Stenosis Severity in EverydaY Practice): A Multicenter Study in Consecutive Patients. J Am Coll Cardiol. 2013; 61:1421–1427.8. Mamas MA, Horner S, Welch E, et al. Resting Pd/Pa measured with intracoronary pressure wire strongly predicts fractional flow reserve. J Invasive Cardiol. 2010; 22:260–265.9. Tonino PA, DeBruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009; 360:213–224.10. De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012; 367:991–1001.11. Jung HO, Seung KB, Kim PJ, et al. Comparison between nicorandil and adenosine in the measurement of coronary flow reserve using a Doppler guide wire. Korean Circ J. 2002; 32:391–397.12. Jang HJ, Koo BK, Lee HS, et al. Safety and efficacy of a novel hyperaemic agent, intracoronary nicorandil, for invasive physiological assessments in the cardiac catheterization laboratory. Eur Heart J. 2013; [Epub ahead of print].13. Lindstaedt M, Bojara W, Holland-Letz T, et al. Adenosine-induced maximal coronary hyperemia for myocardial fractional flow reserve measurements: comparison of administration by femoral venous versus antecubital venous access. Clin Res Cardiol. 2009; 98:717–723.14. De Bruyne B, Pijls NH, Barbato E, et al. Intracoronary and intravenous adenosine 5'-triphosphate, adenosine, papaverine, and contrast medium to assess fractional flow reserve in humans. Circulation. 2003; 107:1877–1883.15. Seo MK, Koo BK, Kim JH, et al. Comparison of hyperemic efficacy between central and peripheral venous adenosine infusion for fractional flow reserve measurement. Circ Cardiovasc Interv. 2012; 5:401–405.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Myocardial Fractional and Coronary Flow Reserve after Revascularization in Acute Myocardial Infarction
- Clinical Implications of Non-Hyperemic Pressure Ratios
- Myocardial fractional flow reserve in acute myocardial infarction
- Clinical Comparison of Coronary Flow Reserve and Fractional Flow Reserve after PTCA in Patients with Coronary Artery Disease
- How to Apply Physiology-Guided Percutaneous Coronary Intervention Optimization?: Theory and Practice