Korean Circ J.
2013 Aug;43(8):565-568. 10.4070/kcj.2013.43.8.565.
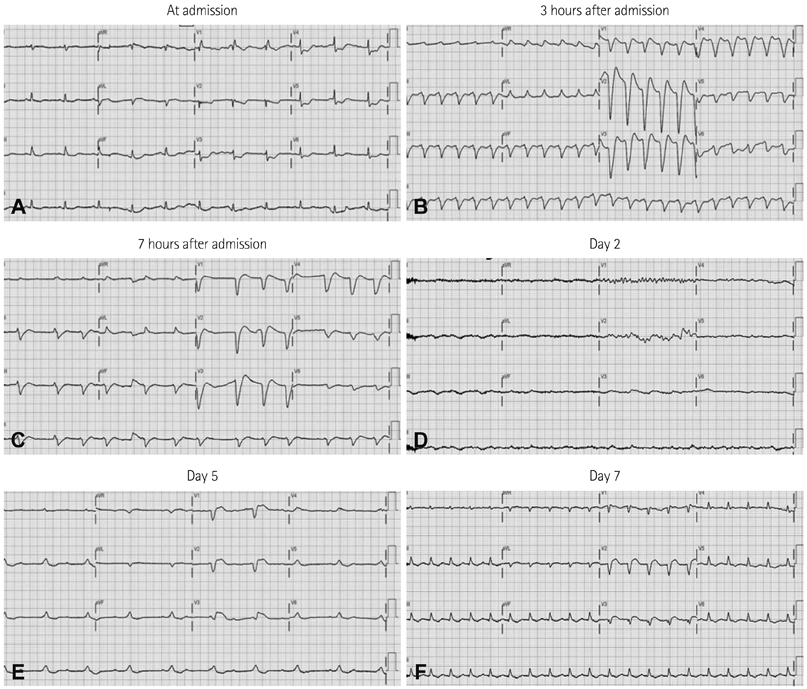
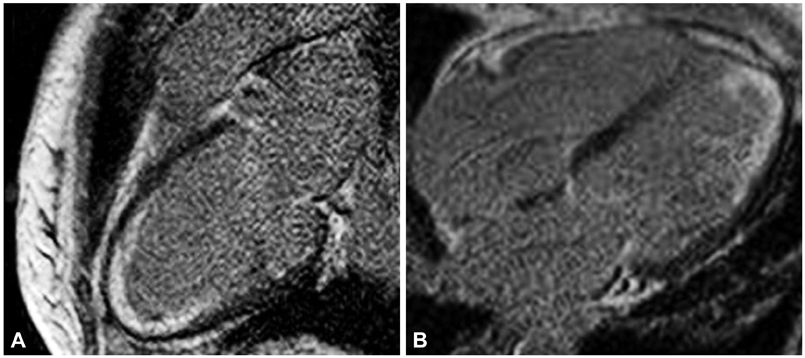
A Case of Reversible Very Low Voltage Electrocardiogram in Fulminant Myocarditis
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. whitesh@catholic.ac.kr
- 2Cardiovascular Center and Cardiology Division, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea.
- 3Cardiovascular Center and Cardiology Division, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2224848
- DOI: http://doi.org/10.4070/kcj.2013.43.8.565
Abstract
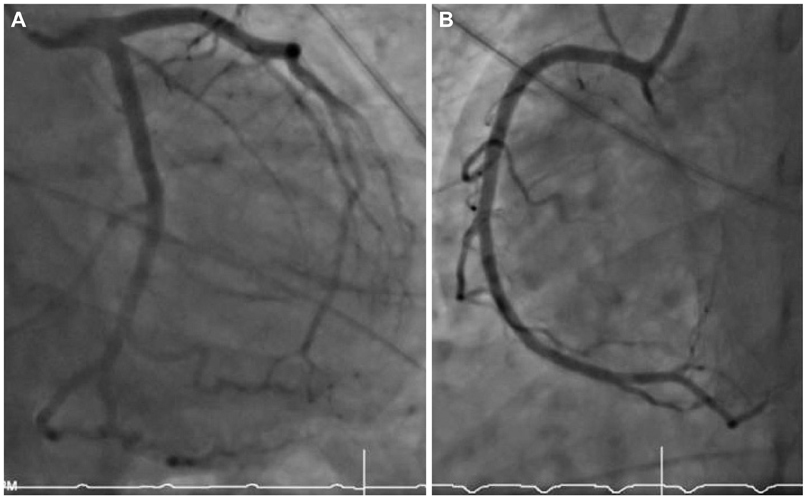
- Clinical features of acute myocarditis range from a subclinical state to a fulminant state. Fulminant myocarditis with ventricular arrhythmia or atrioventricular block is associated with a high mortality rate. In cases in which aggressive medical therapy for fulminant myocarditis is not likely to be successful, intensive and emergency mechanical circulatory support, such as extracorporeal membrane oxygenation (ECMO) or intra-aortic balloon pump, should be considered. We report life salvage of acute fulminant myocarditis in a 53-year-old woman presented with malignant arrhythmia and cardiogenic shock supported by ECMO.
MeSH Terms
Figure
Reference
-
1. Feldman AM, McNamara D. Myocarditis. N Engl J Med. 2000; 343:1388–1398.2. Morgera T, Di Lenarda A, Dreas L, et al. Electrocardiography of myocarditis revisited: clinical and prognostic significance of electrocardiographic changes. Am Heart J. 1992; 124:455–467.3. Bruch C, Schmermund A, Dagres N, et al. Changes in QRS voltage in cardiac tamponade and pericardial effusion: reversibility after pericardiocentesis and after anti-inflammatory drug treatment. J Am Coll Cardiol. 2001; 38:219–226.4. Hare JM, Baughman KL. Fulminant and acute lymphocytic myocarditis: the prognostic value of clinicopathological classification. Eur Heart J. 2001; 22:269–270.5. McCarthy RE 3rd, Boehmer JP, Hruban RH, et al. Long-term outcome of fulminant myocarditis as compared with acute (nonfulminant) myocarditis. N Engl J Med. 2000; 342:690–695.6. Aoyama N, Izumi T, Hiramori K, et al. National survey of fulminant myocarditis in Japan: therapeutic guidelines and long-term prognosis of using percutaneous cardiopulmonary support for fulminant myocarditis (special report from a scientific committee). Circ J. 2002; 66:133–144.7. Marasco SF, Lukas G, McDonald M, McMillan J, Ihle B. Review of ECMO (extra corporeal membrane oxygenation) support in critically ill adult patients. Heart Lung Circ. 2008; 17:Suppl 4. S41–S47.8. Slaughter MS, Rogers JG, Milano CA, et al. Advanced heart failure treated with continuous-flow left ventricular assist device. N Engl J Med. 2009; 361:2241–2251.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Acute Fulminant Myocarditis Progressed into and Recovered from Congestive Heart Failure and Multiorgan Failure
- Percutaneous Extracorporeal Membrane Oxygenation (ECMO) for Acute Fulminant Myocarditis
- A Case of Fulminant Type 1 Diabetes with Pulmonary Hypertension
- Giant Cell Myocarditis Manifested as Fulminant Myocarditis
- Life-Threatening Acute Fulminant Myocarditis Following a Coffee Diet Program