Korean Circ J.
2013 Nov;43(11):770-773. 10.4070/kcj.2013.43.11.770.
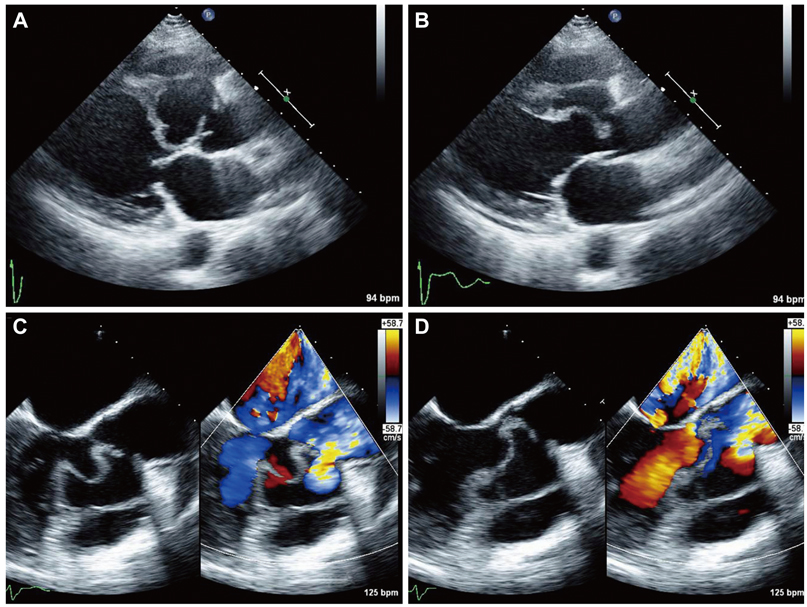
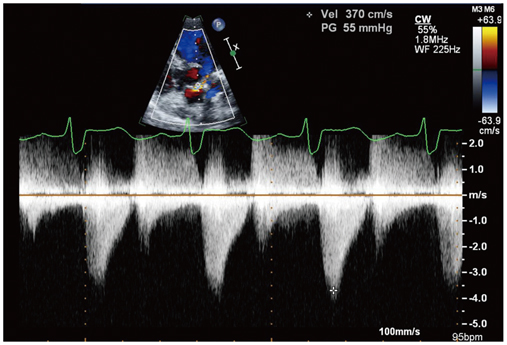
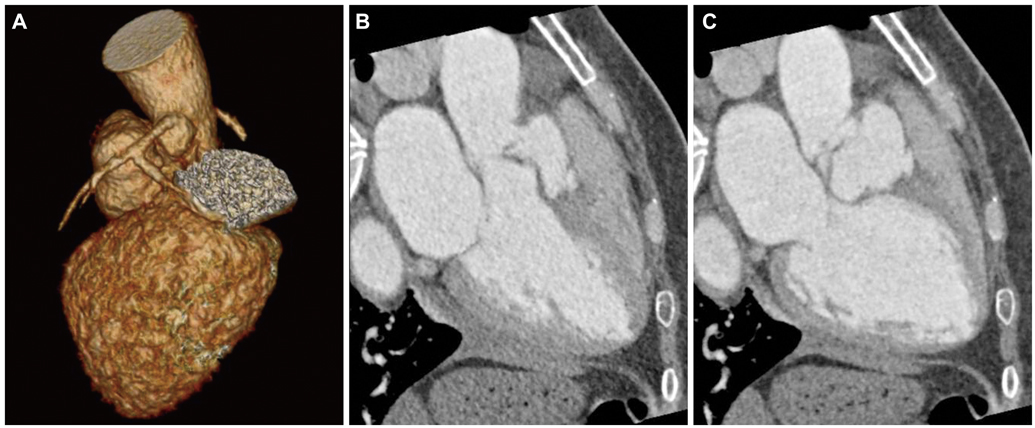
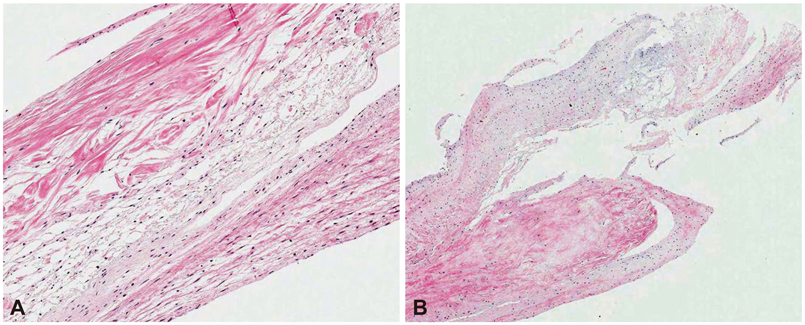
A Case of Right Sinus of Valsalva Rupture with Dissection into Interventricular Septum Causing Left Ventricular Outflow Tract Obstruction
- Affiliations
-
- 1Department of Cardiology, Dong-A University College of Medicine, Busan, Korea. kimyd@dau.ac.kr
- 2Department of Radiology, Dong-A University College of Medicine, Busan, Korea.
- 3Department of Thoracic and Cardiovascular Surgery, Dong-A University College of Medicine, Busan, Korea.
- 4Department of Pathology, Dong-A University College of Medicine, Busan, Korea.
- KMID: 2224810
- DOI: http://doi.org/10.4070/kcj.2013.43.11.770
Abstract
- Sinus of Valsalva aneurysm (SVA) is an uncommon anomaly of the aorta. Rupture of SVA often precipitates dramatic clinical complications, including heart failures. Right SVAs are the most common type, and when they rupture, they usually rupture into the right ventricle or right atrium. Rupture into left ventricle or interventricular septum is rare. Herein, we report a case of right SVA rupture with dissection into interventricular septum, which produced significant left ventricular outflow tract obstruction and aortic regurgitation. The case was successfully treated by surgical operation.
MeSH Terms
Figure
Reference
-
1. Bricker AO, Avutu B, Mohammed TL, et al. Valsalva sinus aneurysms: findings at CT and MR imaging. Radiographics. 2010; 30:99–110.2. Pepper C, Munsch C, Sivananthan UM, Pye M. Unruptured aneurysm of the left sinus of Valsalva extending into the left ventricular outflow tract: presentation and imaging. Heart. 1998; 80:190–193.3. Avci A, Akcakoyun M, Alizada E, et al. Severe right ventricular outflow obstruction by right sinus of valsalva aneurysm. Echocardiography. 2010; 27:341–343.4. Feldman DN, Roman MJ. Aneurysms of the sinuses of Valsalva. Cardiology. 2006; 106:73–81.5. Taher T, Singal R, Sonnenberg B, Ross D, Graham M. Images in cardiovascular medicine. Sinus of valsalva rupture with dissection into the interventricular septum: diagnosis by echocardiography and magnetic resonance imaging. Circulation. 2005; 111:e101–e102.6. Nunes Mdo C, Gelape CL, Barbosa FB, et al. Sinus of valsalva aneurysm with dissection into the interventricular septum. Echocardiography. 2008; 25:102–104.7. Das KM, El-Menyar AA, Arafa SE, Suwaidi JA. Intracardiac shunting of ruptured Sinus of Valsalva aneurysm in a patient presented with acute myocardial infarction: role of 64-slice MDCT. Int J Cardiovasc Imaging. 2006; 22:797–802.8. Park KH, Shin DG, Son CW, et al. Aneurysm of sinus of valsalva dissecting into the interventricular septum after aortic valve replacement: diagnosis by echocardiography and magnetic resonance imaging and treatment with surgical sealant. Korean Circ J. 2011; 41:464–468.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Rare Case of Unruptured Sinus of Valsalva Aneurysm Obstructing the Right Ventricular Outflow Tract
- A Case of Unruptured Aneurysm of the Right Sinus of Valsalva with Right Ventricular Outflow Obstruction
- Two cases of ruptured congenital sinus of Valsalva aneurysms dissecting into the interventricular septum in patients with cerebral infarction
- Aneurysm of Sinus of Valsalva Dissecting Into the Interventricular Septum After Aortic Valve Replacement: Diagnosis by Echocardiography and Magnetic Resonance Imaging and Treatment With Surgical Sealant
- Anomaly of the Left Anterior Descending Coronary Artery Arising from the Right Sinus of Valsalva and Ventricular Septal Defect in Adult: A Rare Case