Korean Circ J.
2015 Sep;45(5):428-431. 10.4070/kcj.2015.45.5.428.
Brachial Plexus Injury Caused by Indwelling Axillary Venous Pacing Leads
- Affiliations
-
- 1Department of Cardiology, Dong-A University Medical Center, Busan, Korea. thinkmed@dau.ac.kr
- 2Department of Cardiovascular Surgery, Dong-A University Medical Center, Busan, Korea.
- 3Department of Radiology, Dong-A University Medical Center, Busan, Korea.
- KMID: 2223808
- DOI: http://doi.org/10.4070/kcj.2015.45.5.428
Abstract
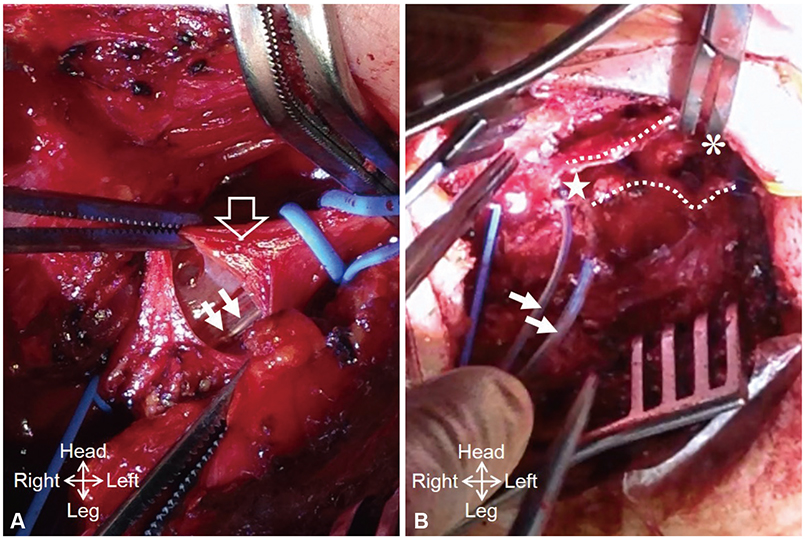
- A 64-year-old male patient underwent cardiac resynchronization therapy (CRT) device implantation via the axillary venous approach. Two weeks later, the patient started complaining of "electric shock-like" pain in the left axillary area. During physical examination, typical pain in the left axillary area was reproduced whenever his left shoulder was passively abducted more than 60 degrees. Fluoroscopic examination showed that the left ventricle (LV) and right atrium (RA) leads were positioned at an acute angle directing towards the left brachial plexus whenever the patient's shoulder was passively abducted. Brachial plexus irritation by the angulated CRT leads was strongly suspected. To relieve the acute angulation, we had to adjust the entry site of the LV and RA leads from the distal to the proximal axillary vein using the cut-down method. After successful lead repositioning, the neuropathic pain improved rapidly. Although transvenous pacing lead-induced nerve injury is not a frequent complication, this possibility should be kept in mind by the operators.
Keyword
MeSH Terms
Figure
Reference
-
1. Kim KH, Park KM, Nam GB, et al. Comparison of the axillary venous approach and subclavian venous approach for efficacy of permanent pacemaker implantation. 8-Year follow-up results. Circ J. 2014; 78:865–871.2. Pozo E, González-Ferrer JJ, Pérez Villacastín J, Macaya C. Diaphragm paralysis due to pseudoaneurysm of internal mammary artery after pacemaker implantation. Europace. 2011; 13:592–593.3. Harris K, Maniatis G, Siddiqui F, Maniatis T. Phrenic nerve injury and diaphragmatic paralysis following pacemaker pulse generator replacement. Heart Lung. 2013; 42:65–66.4. Ramza BM, Rosenthal L, Hui R, et al. Safety and effectiveness of placement of pacemaker and defibrillator leads in the axillary vein guided by contrast venography. Am J Cardiol. 1997; 80:892–896.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Proximal Median Neuropathy Caused by Axillary Brachial Plexus Block
- Persistent Brachial Plexus Injury Associated with Axillary Brachial Plexus Block: A case report
- Brachial Plexus Injury Following Axillary Brachial Plexus Block Using a Transarterial Approach: A case report
- Continuous Brachial Plexus Block as a Treatment for Intractable Pain Management of Malignancy Involving in Brachial Plexus: A report of 3 cases
- Steroid Injection into the Compartment of the Brachial Plexus in a Pediatric Patient with Traumatic Brachial Plexus Injury: A case report