Korean Circ J.
2015 Sep;45(5):391-397. 10.4070/kcj.2015.45.5.391.
Clinical Characteristics and Features of Frequent Idiopathic Ventricular Premature Complexes in the Korean Population
- Affiliations
-
- 1Division of Cardiology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. kyongmin.park@gmail.com
- KMID: 2223803
- DOI: http://doi.org/10.4070/kcj.2015.45.5.391
Abstract
- BACKGROUND AND OBJECTIVES
Frequent ventricular premature complexes (VPCs) increase the risk of cardiomyopathy (CMP). However, most data regarding VPCs have been obtained from Western population and in-hospital patient-based studies. The objective of this study was to define the clinical characteristics and features of idiopathic VPCs in the Korean population.
SUBJECTS AND METHODS
We investigated subjects undergoing transthoracic echocardiography and documented VPC burdens >1% by Holter monitoring in an outpatient clinic at Samsung Medical Center, Korea. We analyzed demographic and clinical features and the nature of the VPCs by electrocardiography (ECG).
RESULTS
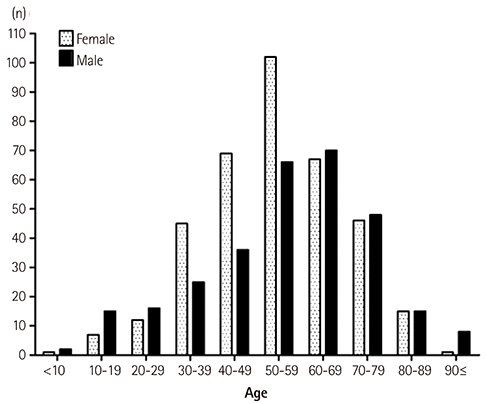
A total of 666 patients were registered. Mean age was 54.7+/-16.8 years, and 365 (54.8%) patients were female. Typical VPC-related symptoms, such as palpitation and a dropped beat, were observed in 394 (59.2%) patients. Some patients received beta-blockers (n=95; 14.3%) and anti-arrhythmic agents (n=14; 2.1%). The ECG analysis was performed in 405 patients; 322 (79.5%) exhibited left bundle branch block (LBBB) and 347 (85.8%) exhibited an inferior axis. The precordial R-wave transition was predominantly distributed over V3 in 230 patients (56.6%). Thirty-one patients (4.5%) were diagnosed with VPC-induced CMP.
CONCLUSION
The incidence of frequent VPCs was slightly higher in females, and palpitation was the most frequent complaint. The most common ECG features were LBBB, inferior axis, and late precordial R-wave transition.
MeSH Terms
Figure
Reference
-
1. Cheriyath P, He F, Peters I, et al. Relation of atrial and/or ventricular premature complexes on a two-minute rhythm strip to the risk of sudden cardiac death (the Atherosclerosis Risk in Communities [ARIC] study). Am J Cardiol. 2011; 107:151–155.2. Simpson RJ Jr, Cascio WE, Schreiner PJ, Crow RS, Rautaharju PM, Heiss G. Prevalence of premature ventricular contractions in a population of African American and white men and women: the Atherosclerosis Risk in Communities (ARIC) study. Am Heart J. 2002; 143:535–540.3. Chugh SS, Shen WK, Luria DM, Smith HC. First evidence of premature ventricular complex-induced cardiomyopathy: a potentially reversible cause of heart failure. J Cardiovasc Electrophysiol. 2000; 11:328–329.4. Ataklte F, Erqou S, Laukkanen J, Kaptoge S. Meta-analysis of ventricular premature complexes and their relation to cardiac mortality in general populations. Am J Cardiol. 2013; 112:1263–1270.5. Bogun F, Crawford T, Reich S, et al. Radiofrequency ablation of frequent, idiopathic premature ventricular complexes: comparison with a control group without intervention. Heart Rhythm. 2007; 4:863–867.6. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005; 18:1440–1463.7. Writing Committee members. Yancy CW, Jessup M, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013; 128:e240–e327.8. Hancock EW, Deal BJ, Mirvis DM, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part V: electrocardiogram changes associated with cardiac chamber hypertrophy: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol. 2009; 53:992–1002.9. Ng GA. Treating patients with ventricular ectopic beats. Heart. 2006; 92:1707–1712.10. Del Carpio Munoz F, Syed FF, Noheria A, et al. Characteristics of premature ventricular complexes as correlates of reduced left ventricular systolic function: study of the burden, duration, coupling interval, morphology and site of origin of PVCs. J Cardiovasc Electrophysiol. 2011; 22:791–798.11. Baman TS, Lange DC, Ilg KJ, et al. Relationship between burden of premature ventricular complexes and left ventricular function. Heart Rhythm. 2010; 7:865–869.12. Yokokawa M, Kim HM, Good E, et al. Impact of QRS duration of frequent premature ventricular complexes on the development of cardiomyopathy. Heart Rhythm. 2012; 9:1460–1464.13. Ban JE, Park HC, Park JS, et al. Electrocardiographic and electrophysiological characteristics of premature ventricular complexes associated with left ventricular dysfunction in patients without structural heart disease. Europace. 2013; 15:735–741.14. Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998; 97:1837–1847.15. Kostis JB, Byington R, Friedman LM, Goldstein S, Furberg C. Prognostic significance of ventricular ectopic activity in survivors of acute myocardial infarction. J Am Coll Cardiol. 1987; 10:231–242.16. Movsowitz C, Schwartzman D, Callans DJ, et al. Idiopathic right ventricular outflow tract tachycardia: narrowing the anatomic location for successful ablation. Am Heart J. 1996; 131:930–936.17. Kamakura S, Shimizu W, Matsuo K, et al. Localization of optimal ablation site of idiopathic ventricular tachycardia from right and left ventricular outflow tract by body surface ECG. Circulation. 1998; 98:1525–1533.18. Kanagaratnam L, Tomassoni G, Schweikert R, et al. Ventricular tachycardias arising from the aortic sinus of valsalva: an under-recognized variant of left outflow tract ventricular tachycardia. J Am Coll Cardiol. 2001; 37:1408–1414.19. Dixit S, Gerstenfeld EP, Callans DJ, Marchlinski FE. Electrocardiographic patterns of superior right ventricular outflow tract tachycardias: distinguishing septal and free-wall sites of origin. J Cardiovasc Electrophysiol. 2003; 14:1–7.20. Callans DJ, Menz V, Schwartzman D, Gottlieb CD, Marchlinski FE. Repetitive monomorphic tachycardia from the left ventricular outflow tract: electrocardiographic patterns consistent with a left ventricular site of origin. J Am Coll Cardiol. 1997; 29:1023–1027.21. Lin D, Ilkhanoff L, Gerstenfeld E, et al. Twelve-lead electrocardiographic characteristics of the aortic cusp region guided by intracardiac echocardiography and electroanatomic mapping. Heart Rhythm. 2008; 5:663–669.22. Betensky BP, Park RE, Marchlinski FE, et al. The V(2) transition ratio: a new electrocardiographic criterion for distinguishing left from right ventricular outflow tract tachycardia origin. J Am Coll Cardiol. 2011; 57:2255–2262.23. Carballeira Pol L, Deyell MW, Frankel DS, et al. Ventricular premature depolarization QRS duration as a new marker of risk for the development of ventricular premature depolarization-induced cardiomyopathy. Heart Rhythm. 2014; 11:299–306.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ventricular premature complexes and associated factors in the early postinfarction period
- Clinical Study of Antiarrhythmic Effect of Mexiletine
- The Effect of Oral Mexiletine on Ventricular Arrhythmias Evaluation by Holter Monitoring
- Risperidone-induced Ventricular Premature C omplexes: A Case Report
- Radiofrequency Ablation of Recurrent Ventricular Premature Complex Originating from near Left Ventricular Summit Guided by Intracardiac Echocardiography