J Rhinol.
2015 Nov;22(2):82-88. 10.18787/jr.2015.22.2.82.
Practice Patterns in Endoscopic Sinus Surgery: Survey of the Korean Rhinologic Society
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Samsung Seoul Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Otorhinolaryngology-Head and Neck Surgery, St. Vincent's Hospital, The Catholic University of Korea, College of Medicine, Seoul, Korea. yp@catholic.ac.kr
- KMID: 2223202
- DOI: http://doi.org/10.18787/jr.2015.22.2.82
Abstract
- BACKGROUND AND OBJECTIVES
Endoscopic sinus surgery (ESS) has become the standard treatment modality in chronic rhinosinusitis. However there is no uniform treatment protocol regarding preoperative, intraoperative, and postoperative care. The objectives of this study are to identify and report the practice patterns of ESS in South Korea. MATERIALS AND METHOD: A series of eight surveys were sent to the board members of the Korean Rhinologic Society via e-mail between August 2013 and September 2014. Responses to questions regarding detailed practice patterns were recorded anonymously.
RESULTS
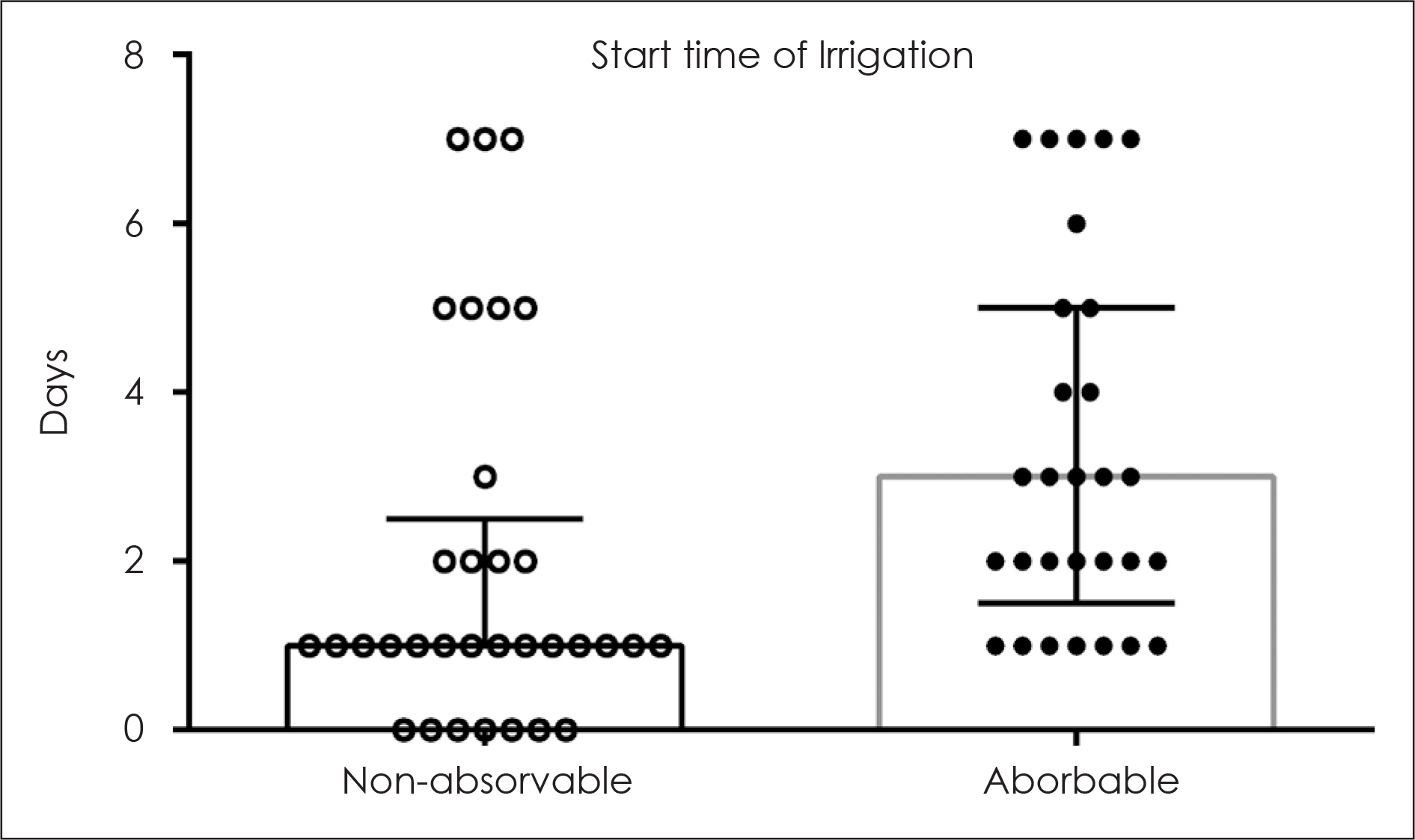
The average number of replies to each survey was 41.5. Routine antibiotics were prescribed just before computed tomography by 46.9% of the respondents, and the mean duration of antibiotics treatment was 1.90 weeks. A routine preoperative olfactory test was conducted by 64.3% of respondents, and allergy tests were conducted by 82.2%. General anesthesia was preferred by 76.8%, and the mean hospitalization period was 3.12 days. The mean rotation speed used for a microdebrider was 3,054 rpm, and 3,000 rpm was selected by 51.6% of the respondents. In addition, 74.2% of respondents reported that they operate the foot switch themselves. Finally, an absorbable pack was preferred after ESS.
CONCLUSION
The current study was the first nationwide survey on practice patterns in endoscopic sinus surgery in Korea, and the data reflects the opinions of expert sinus surgeons.
Keyword
MeSH Terms
Figure
Reference
-
References
1). Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology. 2012; 50(1):1–12.
Article2). 국민건강보험공단;2013. 주요수술통계연보. 2014.3). Lanza DC, Kennedy DW. Current concepts in the surgical management of chronic and recurrent acute sinusitis. J Allergy Clin Immunol. 1992; 90(3 Pt 2):505–10. discussion 11.
Article4). Park JH, Lee SD, Lee JH, Lee YB. Functional Endoscopic Sinus Surgery in Chronic Paranasal Sinusitis. Korean J Otolaryngol. 1994; 37(4):725.5). Setliff RC 3rd. The hummer: a remedy for apprehension in functional endoscopic sinus surgery. Otolaryngol Clin North Am. 1996; 29(1):95–104.
Article6). Hepworth EJ, Bucknor M, Patel A, Vaughan WC. Nationwide survey on the use of imageguided functional endoscopic sinus surgery. Otolaryngol Head Neck Surg. 2006; 135(1):68–73.
Article7). Portela RA, Hootnick J, McGinn J. Perioperative care in functional endoscopic sinus surgery: a survey study. Int Forum Allergy Rhinol. 2012; 2(1):27–33.
Article8). Gonzalez-Castro J, Pascual J, Busquets J. National survey on the use of preoperative systemic steroids in endoscopic sinus surgery. Int Forum Allergy Rhinol. 2013; 3(6):497–503.9). Smith EJ, Stringer S. Current perioperative practice patterns for minimizing surgical site infection during rhinologic procedures. Int Forum Allergy Rhinol. 2014; 4(12):1002–7.
Article10). Soudry E, Mohabir PK, Miglani A, Chen J, Nayak JV, Hwang PH. Outpatient endoscopic sinus surgery in cystic fibrosis patients: predictive factors for admission. Int Forum Allergy Rhinol. 2014; 4(5):416–21.
Article11). Thomas JG, Gadgil N, Samson SL, Takashima M, Yoshor D. Prospective trial of a short hospital stay protocol after endoscopic endonasal pituitary adenoma surgery. World Neurosurg. 2014; 81(3–4):576–83.
Article12). Hobson CE, Choby GW, Wang EW, Morton SC, Lee S. Systematic review and metaanalysis of middle meatal packing after endoscopic sinus surgery. Am J Rhinol Allergy. 2015; 29(2):135–40.
Article13). Suzuki C, Nakagawa T, Yao W, Sakamoto T, Ito J. The need for intranasal packing in endoscopic endonasal surgery. Acta Otolaryngol Suppl 2010 (563):. 39–42.14). Freeman SR, Sivayoham ES, Jepson K, de Carpentier J. A preliminary randomised controlled trial evaluating the efficacy of saline douching following endoscopic sinus surgery. Clin Otolaryngol. 2008; 33(5):462–5.
Article15). Rudmik L, Soler ZM, Orlandi RR, Stewart MG, Bhattacharyya N, Kennedy DW, et al. Early postoperative care following endoscopic sinus surgery: an evidence-based review with recommendations. Int Forum Allergy Rhinol. 2011; 1(6):417–30.
Article16). Macdonald KI, Wright ED, Sowerby LJ, Rotenberg BW, Chin CJ, Rudmik L, et al. Squeeze bottle versus saline spray after endoscopic sinus surgery for chronic rhinosinusitis: a pilot multicentre trial. Am J Rhinol Allergy. 2015; 29(1):13–7.
Article17). Snidvongs K, Pratt E, Chin D, Sacks R, Earls P, Harvey RJ. Corticosteroid nasal irrigations after endoscopic sinus surgery in the management of chronic rhinosinusitis. Int Forum Allergy Rhinol. 2012; 2(5):415–21.
Article18). Jang DW, Lachanas VA, Segel J, Kountakis SE. Budesonide nasal irrigations in the postoperative management of chronic rhinosinusitis. Int Forum Allergy Rhinol. 2013; 3(9):708–11.
Article19). Lee JT, Chiu AG. Topical anti-infective sinonasal irrigations: update and literature review. Am J Rhinol Allergy. 2014; 28(1):29–38.
Article20). Rudmik L, Hoy M, Schlosser RJ, Harvey RJ, Welch KC, Lund V, et al. Topical therapies in the management of chronic rhinosinusitis: an evidence-based review with recommendations. Int Forum Allergy Rhinol. 2013; 3(4):281–98.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Survey on the Management of Chronic Rhinosinusitis in the Korean Rhinologic Society
- Headache Characteristics in Rhinologic Patients and the Role of Surgical Treatment
- Isolated Inverted Papilloma of the Sphenoid Sinus Presenting as Ptosis
- Endoscopic Frontal Sinus Surgery
- Headache and Facial Pain in Rhinologic Field : A 1 Year Experience